I do not believe it is airborn it is touch
2 posters
Page 1 of 3
Page 1 of 3 • 1, 2, 3 
 Re: I do not believe it is airborn it is touch
Re: I do not believe it is airborn it is touch
https://www.nytimes.com/2023/04/30/opinion/masks-pandemic.html
The Next Pandemic
OPINION
How Well Does Masking Work? And Other Pandemic Questions We Need to Answer.
The Next Pandemic
OPINION
How Well Does Masking Work? And Other Pandemic Questions We Need to Answer.
By Jennifer B. Nuzzo
Dr. Nuzzo is the director of the Pandemic Center at Brown University School of Public Health.
You’re reading The Next Pandemic newsletter. Insights and guidance for preparing for future outbreaks.
When the coronavirus took off in 2020, the unknowns were immense, as was the urgency. It was clear that the virus was novel, that it was spreading widely and that it was killing many of the people it infected. And there was no vaccine or proven drug treatment. This was the context in which states first mandated masks, issued stay-at-home orders and closed schools, among other measures — an emergency.
But now we should have more data from this pandemic to guide our decisions. We don’t send rockets into space without collecting data to monitor their progress and detect if they are veering off course. And yet we witnessed more than one million Covid-19 deaths in the United States without a clear plan to assess whether we were doing all we could to prevent more.
We should be systematically studying pandemic mitigation efforts in order to learn which interventions are effective and how best to employ them. Just as important: We should do so with the understanding that the absence of evidence of effectiveness is not the same as having evidence of ineffectiveness.
Questions about masking, for example, were recently revived by a Cochrane study reporting that masking (with surgical ones or respirators like N95) makes “little or no difference” in reducing infection at the population level, such as among health care workers or in communities. Some mask opponents claim this validates their assertions that masks don’t work. Some mask supporters are raising questions about the study’s authors and attempting to discredit their conclusions. Which side is right?
ADVERTISEMENT
Continue reading the main story
As with most things about the Covid pandemic, the answer is most likely somewhere in between.
There is good evidence that masks can protect people who use them correctly and consistently. Laboratory studies clearly show that wearing a mask properly, when in the presence of the virus, will reduce a person’s exposure to it. Other studies show that higher-quality masks, such as N95 respirators, are better able to keep the virus out than less well-fitting surgical masks or cloth masks.
The confusion occurs when we shift from showing that masks work in a laboratory or for individual people to finding evidence that masking works at the population level and what interventions work to encourage it. At the population level, compliance and mask quality may vary, making it difficult to find evidence to review on the effectiveness of masking in reducing the number of respiratory infections. The Cochrane review tried to untangle the evidence in one analysis. And according to that limited evidence, masking at the population level did not have a clear impact on reducing infections.
How can this be? Part of the reason has to do with the quality of studies on masking. Though there have been studies observing differences in disease rates between places with masking policies and those without, evidence from these observational studies isn’t of the highest quality because it doesn’t fully account for other differences between masking and nonmasking populations.
To address the quality issue of these studies, the Cochrane review looked only at randomized trials evaluating the effectiveness of masking. Randomized trials are particularly helpful for studying the impact of health interventions within populations because they help to minimize bias and confusion caused by other factors besides the one you are trying to evaluate. For example, if you looked at infections among people who choose to mask versus those who don’t, you may be observing not just the effect of masking but also the effects of other protective decisions that people who are inclined to mask may also take, such as avoiding crowded indoor spaces.
There have been only a few randomized trials specific to masking, and most of the ones included in the Cochrane review were not conducted during the Covid-19 pandemic or in the United States. Many of the studies that the Cochrane review included looked at the spread of influenza.
Editors’ Picks
Looted Monastery Manuscripts Rediscovered During Office Renovation
Everything You Need to Know About the 2023 Met Gala
The Weekend-Only Exercise Plan
ADVERTISEMENT
Continue reading the main story
This is important because while we think there are some similarities between how the novel coronavirus and other respiratory viruses are spread, there also are likely to be important differences. Covid proved to be deadlier than seasonal influenza, which may have influenced how often and well people wore masks. Masking for Covid was also mandated throughout much of the United States, which most likely also influenced masking behavior.
The pertinent question isn’t whether masks work but why masking didn’t prove to be highly effective in the most rigorous studies. Was it because adherence to masking, not the masks themselves, was the problem? Is it because the population studied wore masks when around infected people but then got infected from family members? Maybe people didn’t wear masks properly because they weren’t comfortable or they didn’t fit. Knowing the answers to these questions will help us know how best to use masks and help us better control the spread of infections. The Cochrane review authors say their examination was limited to whether interventions to promote mask wearing help to slow the spread of respiratory viruses. It’s important to note that masks only work when people wear them, so adherence will always be key.
In early 2020, when we knew little about the virus but saw its toll, masks were a reasonable step because they had few harms. Considering the rapid spread of the virus and its deadly impact, we could not wait until we had all the data to understand how best to use them. And if a new, deadly respiratory disease emerged tomorrow, we’d have few tools besides masks to prevent spread and protect ourselves.
But we should have put into place efforts to rapidly collect and assess high-quality data to understand whether masks were having optimal effectiveness and, if not, how to increase that effectiveness. We should have done this for other mitigations, too, like school and business closings and policies that required exposed contacts of cases to quarantine. Pandemic measures like masking and vaccination have been challenged by political leaders and in the courts. Without clear evidence at the population level that mitigation measures meaningfully change transmission rates, it will be harder to meet challenges that could block effective, lifesaving interventions.
ADVERTISEMENT
Continue reading the main story
We need to develop clear plans for randomized and other well-designed studies and get them funded. A review of research by investigators affiliated with U.S. governmental public health entities during the pandemic found very few studies that evaluated the impact of measures to control the spread of disease. It is ludicrous to simply hope academic researchers will spontaneously choose and muster the resources necessary to address the most pressing pandemic response questions. Just as we have established research networks and protocols to conduct the highest-quality evaluations of the effectiveness of vaccines, we should have the same for nonpharmaceutical interventions, like masking. We can and must identify the highest-priority research questions and the funding to systematically and rigorously investigate them.
Read more
Opinion | Zeynep Tufekci
Here’s Why the Science Is Clear That Masks Work
March 10, 2023
Jennifer Nuzzo is the director of the Pandemic Center at Brown University School of Public Health and a senior fellow for global health at the Council on Foreign Relations.
dean- Posts : 5607
Join date : 2008-01-01
 Re: I do not believe it is airborn it is touch
Re: I do not believe it is airborn it is touch
since it was fresh in their minds, we need more details.
this was outdoors.
https://businessinsider.mx/personas-vacunadas-infectan-variante-delta-tras-boda-aire-libre/
6 people got the Delta variant at a wedding despite being vaccinated - those with the Pfizer and Moderna doses survived
this was outdoors.
https://businessinsider.mx/personas-vacunadas-infectan-variante-delta-tras-boda-aire-libre/
6 people got the Delta variant at a wedding despite being vaccinated - those with the Pfizer and Moderna doses survived
dean- Posts : 5607
Join date : 2008-01-01
 Re: I do not believe it is airborn it is touch
Re: I do not believe it is airborn it is touch
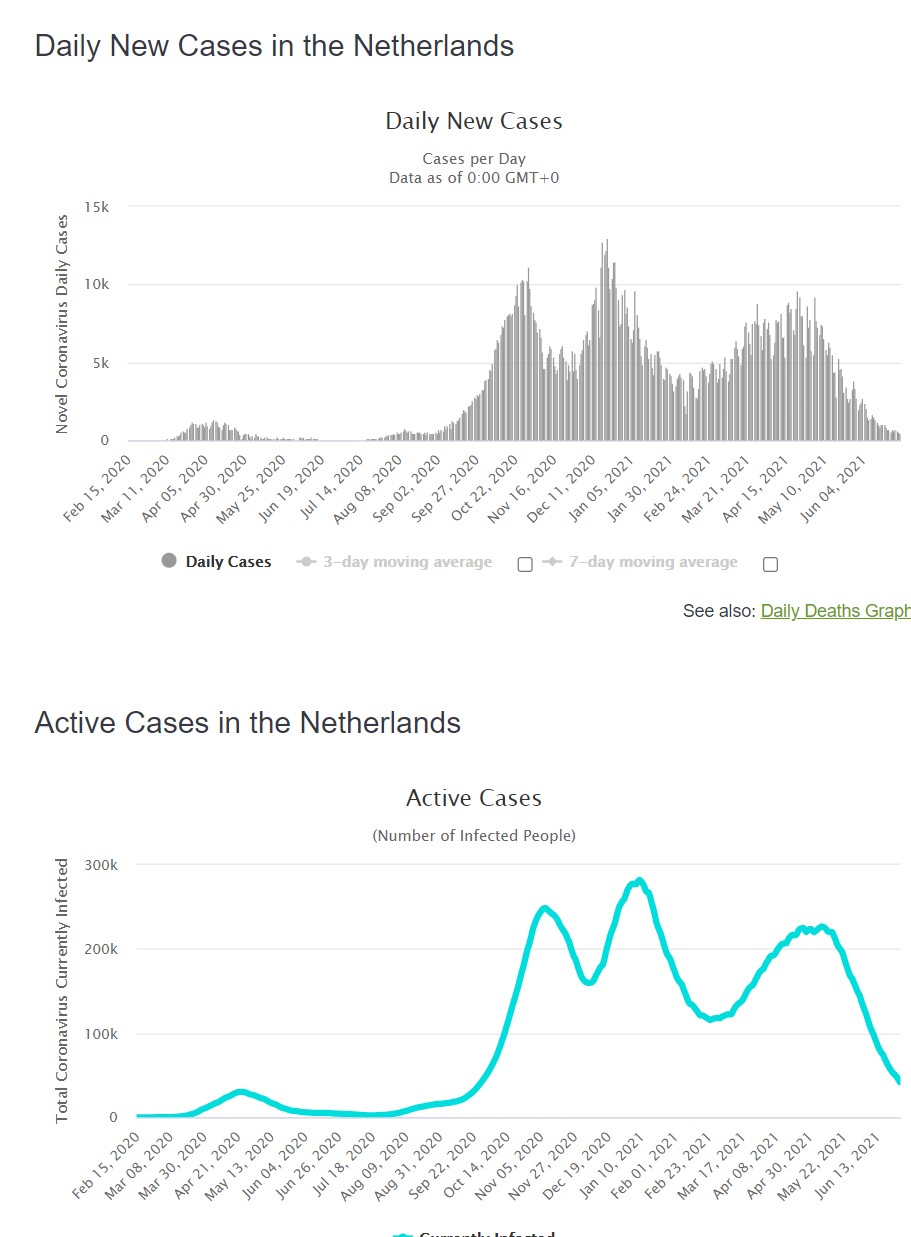
Holland head of the pandemic left the beaches open last year and was the only country in the EU to allow tourism openly. He also believed the virus was not airborne. So masks were not required during the summer and he did put in special cleaning and such requirements for bars, restaurants and coffeshops and so on. They did leave the mandatory masking up to the local cities if they wanted too. And then as winter hit and tourists gone it spiked and put in masking in december 2020, and remove mandatory mask in june 2021
Anyway to me with tourists allowed all things open, no masks required if airborne it would be impossible to explain why they had virtually no cases. But if one says it is contact and they did wash their hands clean common surfaces and most touched surfaces as directed it to me is the obvious proof it is not airborne as the "airborners claim". There is just no reasonable rationale that Holland could have had such a low rate. ya right it was airborne everywhere where people wore masks but not in Holland where they did not.
https://www.straitstimes.com/world/europe/dutch-to-ditch-most-facemask-rules-as-covid-19-cases-fall
Dutch to ditch most face mask rules as Covid-19 cases fall
Anyway to me with tourists allowed all things open, no masks required if airborne it would be impossible to explain why they had virtually no cases. But if one says it is contact and they did wash their hands clean common surfaces and most touched surfaces as directed it to me is the obvious proof it is not airborne as the "airborners claim". There is just no reasonable rationale that Holland could have had such a low rate. ya right it was airborne everywhere where people wore masks but not in Holland where they did not.
https://www.straitstimes.com/world/europe/dutch-to-ditch-most-facemask-rules-as-covid-19-cases-fall
Dutch to ditch most face mask rules as Covid-19 cases fall
https://www.iamexpat.nl/expat-info/dutch-expat-news/face-masks-now-officially-mandatory-netherlands
Face masks now officially mandatory in the Netherlands
Facebook Twitter LinkedIn reddit What's up
01 December 2020, By Victoria Séveno
The government’s controversial and temporary coronavirus law comes into effect on December 1, meaning that face masks are now mandatory in all indoor public spaces in the Netherlands.
The Temporary COVID-19 Measures Act
The Temporary COVID-19 Measures Act will be in place for three months, and allows the Dutch government more power over implementing national coronavirus measures. Under the new law, the government is able to implement a national mandatory face rule.
On top of the face mask rule, the law also turns the ban on singing and shouting in groups into urgent advice, and removes the advice for keeping 1,5-metre distance from other members of your household.
Lastly, the law changes the way in which Prime Minister Mark Rutte introduces new measures. Up until now, any new measures have been implemented as emergency regulation on the instruction of the Minister of Health, Welfare, and Sport (Hugo de Jonge). Now, coronavirus measures proposed by the cabinet must be submitted to the House of Representatives (Tweede Kamer) and Senate (Eerste Kamer) for approval. If the Tweede Kamer doesn’t approve a measure, it cannot be implemented.
Mandatory face mask rule in the Netherlands
While the government has introduced a 95-euro fine for anyone who fails to wear a mask (and who can’t provide evidence of exemption from the rule), the responsibility of enforcing the face mask rule will fall to retailers and business owners. They will not be able to issue fines, but could deny access to their shop or business.
Many shops, including Albert Heijn, HEMA, and Kruidvat, have already announced that they will not deny entry to any customer who refuses to wear a mask. A spokesperson for HEMA said it was up to their members of staff to assess the situation and decide for themselves what action should be taken: “It is mandatory for our staff and we request it from the customers. The staff may talk to the people, refuse them or call someone in like a BOA (Community Service Officer). We don't want it to end in a brawl, that benefits nobody."
Herbert Bruls, chairman of the Security Council, said on Monday that he was disappointed by these announcements: “You cannot say that if a customer enters your store or theatre and does not want to wear a mask that you won’t take action. You are responsible and have to obey the law." Any shop that repeatedly fails to enforce the rule will risk a fine of up to 4.000 euros, or even forced closure.
According to the Dutch government, not wearing a mask will result in police officers or BOAs issuing you a fine, however the chairman of the BOA association, Ruud Kuin, said it will take at least a week or two before any fines will be handed out. There are back-end administration issues that have to be handled before any fines can be issued, he says.
dean- Posts : 5607
Join date : 2008-01-01
 Re: I do not believe it is airborn it is touch
Re: I do not believe it is airborn it is touch
here is a recent peer reviewed science thatis interesting to read how they do not put a definitive to if it is airborne. Only give a probability which could be non-airborne as much as it is. Again the bullet trains in china to me prove to a high degree of certainty since the it was done before mask wearing, and you breath forward and hench should have seen a greater probability of catching covid if airborne. But sitting next to an infected person average time 3.6 percent but if in front 1.8 percent in a 2 hour average timeframe.
Also they referenced a study before masks in a ship, that determined it was absolutely not passed on by the ships ventilation system. https://ehp.niehs.nih.gov/doi/10.1289/EHP7886
Quantitative Microbial Risk Assessment for Airborne Transmission of SARS-CoV-2 via Breathing, Speaking, Singing, Coughing, and Sneezing
the cruise ship
https://www.medrxiv.org/content/10.1101/2020.04.09.20059113v1
Transmission routes of Covid-19 virus in the Diamond Princess Cruise ship
Also they referenced a study before masks in a ship, that determined it was absolutely not passed on by the ships ventilation system. https://ehp.niehs.nih.gov/doi/10.1289/EHP7886
Quantitative Microbial Risk Assessment for Airborne Transmission of SARS-CoV-2 via Breathing, Speaking, Singing, Coughing, and Sneezing
the cruise ship
https://www.medrxiv.org/content/10.1101/2020.04.09.20059113v1
Transmission routes of Covid-19 virus in the Diamond Princess Cruise ship
dean- Posts : 5607
Join date : 2008-01-01
 Re: I do not believe it is airborn it is touch
Re: I do not believe it is airborn it is touch
here they did a full quarinteine on a ship with infected people and in 14 days the only exception that caused further infection was from broken protocol a kettle that was shared which resulted in at least one infection(s).
https://wwwnc.cdc.gov/eid/article/27/5/20-4142_article
Successful Control of an Onboard COVID-19 Outbreak Using the Cruise Ship as a Quarantine Facility, Western Australia
https://wwwnc.cdc.gov/eid/article/27/5/20-4142_article
Successful Control of an Onboard COVID-19 Outbreak Using the Cruise Ship as a Quarantine Facility, Western Australia
A breach of quarantine was reported on day 5 when 3 nEC shared a kettle between adjacent rooms. Subsequently, 1 nEC became symptomatic and tested positive for SARS-CoV-2. A member of the external catering staff reported headache and fever (38°C) on day 7 of quarantine. She tested negative for SARS-CoV-2 and quarantined at home until symptoms resolved.
dean- Posts : 5607
Join date : 2008-01-01
 Re: I do not believe it is airborn it is touch
Re: I do not believe it is airborn it is touch
how do these scientists not connect the dots...
https://www.thelancet.com/journals/laninf/article/PIIS1473-3099(20)30985-3/fulltext
Transmission of COVID-19 in 282 clusters in Catalonia, Spain: a cohort study
Discussion
https://www.thelancet.com/journals/laninf/article/PIIS1473-3099(20)30985-3/fulltext
Transmission of COVID-19 in 282 clusters in Catalonia, Spain: a cohort study
Discussion
In our study, we found that increasing viral load values in nasopharyngeal swabs of patients with COVID-19 were associated with the greater risk of transmission, measured by SARS-CoV-2 PCR positivity among contacts, and with a higher risk of transmission in a household environment compared with that in other indoor situations. Additionally, we found that higher viral loads in swabs of asymptomatic contacts were associated with higher risk of developing symptomatic COVID-19, and that these contacts had shorter incubation periods than those with a lower viral load. Relationships between viral load and infectivity have been described for other respiratory viruses, and our study shows that the same is true for SARS-CoV-2.
To our knowledge, this is the largest study that evaluated the relationship of viral load in patients with COVID-19 and risk of transmission. In our cohort, a high proportion (192 [68%] of 282) of index cases did not cause secondary infections. However, we identified 90 (32%) clusters with transmission events, and the multivariate analysis revealed that clusters centred on index cases with high viral load were significantly more likely to result in transmission. In line with previous analyses of case-contact clusters,9, 12, 14 we also found that household exposure to an index case was associated with a higher risk of transmission than other types of contact, presumably reflecting duration and proximity of exposure. Increasing age of the contact was also identified in our multivariate analysis as a significant–albeit modest–determinant of transmission risk. This factor has shown uneven influence across results reported elsewhere but seems to play a secondary role among adults.13, 14 Finally, unlike previous analyses that reported a relationship between coughing and transmission,13 we did not find any association. This finding suggests that the absence of cough does not preclude significant onward transmission, particularly if the viral load is high. Taken together, our results indicate that the viral load, rather than symptoms, might be the predominant driver of transmission.
Importantly, we report that high viral load shortly after exposure in asymptomatic contacts was strongly associated with the risk of developing symptomatic COVID-19 disease. We found an approximately 40% risk of developing symptomatic disease among individuals with an initial viral load lower than 1 × 107 copies per mL compared with a risk higher than 66% among individuals with a viral load of 1 × 11010 copies per mL or higher. These data might provide rationale for risk stratification for developing illness. Moreover, the initial viral load significantly shifted the incubation time, which ranged from 5 days in participants with a high viral load to 7 days in participants with a low viral load. To our knowledge, our study was the first analysis of prospective data that investigated the association between initial viral load and incubation time.
The study has several limitations. First, asymptomatic people were not enrolled as index cases, affecting our ability to fully characterise all types of transmission chain. Second, we did not find any evidence of decreased risk of transmission in individuals who reported mask use. Although this finding collides with the evidence reported elsewhere,8 we did not have fine-grained data on type of mask (surgical vs FFP2) or use of other measures of personal protective equipment (PPE) or other infection control practices, thus limiting our ability to make clear inferences about the effect of PPE on transmission risk. Mask use is probably correlated with type of exposure, which might further confound associations, but we did not note any association between mask use and risk either in our unadjusted analysis (table 3) or in a multivariable model excluding type of exposure (data not shown). Third, we used time to symptom onset (with later confirmation of infection) rather than time to positive PCR test based on serial testing. Nonetheless, accurate calculation of the incubation period was feasible because of the prospective nature of the study, accurate identification of exposure by face-to-face interview, and intensive active and passive monitoring of exposed contacts. We followed up participants over 14-day periods, thus incubation periods longer than 14 days might not have been detected. Within each cluster, we cannot be completely certain about the directionality of transmission, but our inclusion criteria including the absence of COVID-19-like symptoms in the 2 weeks preceding enrolment is consistent with transmission from a case to a contact. We also cannot exclude that some individuals might have been infected by individuals outside of study clusters but, as per national guidelines, all contacts were quarantined after exposure to index cases, reducing the chance of transmission from elsewhere. Samples were available from index cases a median of 4 days after symptom onset, and the initial sample in contacts was taken on average 5 days after exposure, which might limit our ability to detect associations with peak viral load. Despite this, we still showed clear dose effects in relation to both risk of transmission and time to symptom onset. Finally, our study population is reflective of the trial from which the study sample was drawn and is, therefore, biased towards female participants and participants with few comorbidities and predominantly mild to moderate infection; additional data are needed on the risk of transmission in other populations.
In summary, our results provide evidence regarding the determinants of SARS-CoV-2 transmission, particularly on the role of the viral load. The higher risk of transmission among individuals with higher viral loads adds to existing evidence and encourages the assessment of the viral load in patients with a large number of close contacts. When a patient with high viral load is identified, the implementation of reinforced contact tracing measures and quarantines might be crucial to reduce onward transmission. Similarly, our results regarding the risk and expected time to developing symptomatic COVID-19 encourage risk stratification of newly diagnosed SARS-CoV-2 infections on the basis of initial viral load.
dean- Posts : 5607
Join date : 2008-01-01
 3 foot vs 6 foot
3 foot vs 6 foot
well well some interesting data... 3 foot and 6 foot does not make a difference, if it was truly airbone it certainly would.
https://academic.oup.com/cid/advance-article/doi/10.1093/cid/ciab230/6167856
https://academic.oup.com/cid/advance-article/doi/10.1093/cid/ciab230/6167856
Effectiveness of three versus six feet of physical distancing for controlling spread of COVID-19 among primary and secondary students and staff: A retrospective, state-wide cohort study• Increasing physical distancing requirements in schools from ≥3 feet to ≥6 feet was not associated with a reduction in SARS-CoV-2 cases among students or staff if other mitigation measures were implemented, based on a retrospective cohort study of students (n=537,336) and staff (n=99,390) among 251 school districts with any in-person learning in Massachusetts during the Fall 2020 academic period. 96% of school districts implemented a ≥3 feet distancing policy, 64% of districts reported limiting on-campus enrollment, and all districts adopted universal masking for both students in grade 2 and above and for school staff. After adjusting for race/ethnicity and socio-economic status, there was no difference in the incidence rates between schools with a ≥3 feet vs ≥6 feet distancing policy among students (aIRR=0.761) and staff (aIRR=0.902). Incidence rates in both students and staff were strongly correlated with community incidence and positive cases in schools, particularly among school staff.
dean- Posts : 5607
Join date : 2008-01-01
 Re: I do not believe it is airborn it is touch
Re: I do not believe it is airborn it is touch
these guys are loonies, they do not explain the peer reviewed science I posted here.
https://docs.google.com/document/d/1fB5pysccOHvxphpTmCG_TGdytavMmc1cUumn8m0pwzo/edit
https://indoor-covid-safety.herokuapp.com/
https://docs.google.com/document/d/1fB5pysccOHvxphpTmCG_TGdytavMmc1cUumn8m0pwzo/edit
https://indoor-covid-safety.herokuapp.com/
dean- Posts : 5607
Join date : 2008-01-01
 masks and barriers made no difference in several plants
masks and barriers made no difference in several plants
wow oh wow, see what happens when you have been made prejudice. Look at this is airborne here is a food processing study with before and after. Before masks and plexiglas seperations. Yet they admit and then claim it is small particles must be getting away from them. In this study where they had implimented mask wearing and plexiglass to seperate workers at their work location and in the lunchroom. They admit in one factory the rate went up and in some others being studied there was no change in rate. IE in 62 percent of the factories the numbers went down. So that leaves with those precautions 38% it made no difference or got worse. I call BS to their theory not proven by any study to this date that was objective. Again it was contact and they did not focus into stopping cross contact.
https://wwwnc.cdc.gov/eid/article/27/4/20-4800_article?mkt_tok=eyJpIjoiTlRVeVpXUXlOamRoTldOaSIsInQiOiJMelwvUFNtTXZIZytBNk1UU3lwWWkzZ2hvc3ZMMnVHd2xXSHQxSVwvNnRpVmhWXC9cL1kwSVhMTHlPcGQ0eHBJaEI1WjZGd0lBNDZUUHloTVBhMEo3OUVWWjF0azg1eFplTXFKc1lOUThcL1E3RDZpZmtYV0VJSFN4UHErYUpCcDFBekl6In0%3D
Characteristics of SARS-CoV-2 Transmission among Meat Processing Workers in Nebraska, USA, and Effectiveness of Risk Mitigation Measures
https://wwwnc.cdc.gov/eid/article/27/4/20-4800_article?mkt_tok=eyJpIjoiTlRVeVpXUXlOamRoTldOaSIsInQiOiJMelwvUFNtTXZIZytBNk1UU3lwWWkzZ2hvc3ZMMnVHd2xXSHQxSVwvNnRpVmhWXC9cL1kwSVhMTHlPcGQ0eHBJaEI1WjZGd0lBNDZUUHloTVBhMEo3OUVWWjF0azg1eFplTXFKc1lOUThcL1E3RDZpZmtYV0VJSFN4UHErYUpCcDFBekl6In0%3D
Characteristics of SARS-CoV-2 Transmission among Meat Processing Workers in Nebraska, USA, and Effectiveness of Risk Mitigation Measures
Our results indicate significantly reduced incidence of COVID-19 cases in 62% of studied facilities following adoption of universal masking and physical barrier interventions. Several factors may explain why some facilities did not see incidence decrease and 1 saw incidence significantly increase after initiating these measures. First, as an engineering control, physical barriers are generally considered one of the most effective measures to reduce person-to-person transmission of a communicable disease because they do not rely on worker adherence (21). However, since the study period, evidence has mounted supporting the substantial role of aerosols in transmitting COVID-19 (22–24). Although physical barriers installed between meat processing workers on the production line and at cafeteria tables would block larger respiratory droplets, the primary mode of transmission according to the CDC (22), they would not fully protect against aerosol transmission. Moreover, low temperatures and limited fresh air supply combined with physically demanding work conditions could facilitate longer-range aerosol transmission (25). Enhancements in ventilation (e.g., increasing the number of air exchanges per hour, installing high efficiency particulate air [HEPA] filtration) should therefore be considered the most effective engineering control for COVID-19. More study is needed on aerosol transmission dynamics in this setting.
Last edited by dean on Sun Feb 21, 2021 8:12 pm; edited 1 time in total
dean- Posts : 5607
Join date : 2008-01-01
 Re: I do not believe it is airborn it is touch
Re: I do not believe it is airborn it is touch
here is an interesting study.
Note that most if not all of these are high contact positions, ie they touch things that others have touched in general. and most are in areas with lots of air volume (example grounds maintenance workers, not near people what so ever) and we can assume most are high mask wearing occupations.
https://finance.yahoo.com/news/jobs-with-the-highest-risk-of-death-in-the-pandemic-193906412.html
Here are the jobs with the largest increase in deaths in the pandemic

dean- Posts : 5607
Join date : 2008-01-01
 Black lives matter protests
Black lives matter protests
I believe the finding of data from Black Lives Matter protests of none being super spreader events also supports it is not airborne. Again these were people yelling at the top of their lungs.
https://ncrc.jhsph.edu/research/black-lives-matter-protests-and-covid-19-cases-relationship-in-two-databases/
https://www.healthline.com/health-news/black-lives-matter-protests-didnt-contribute-to-covid19-surge
https://www.usatoday.com/story/news/factcheck/2020/09/17/fact-check-sturgis-rallys-covid-19-cases-misstated-online-post/3458606001/
https://ncrc.jhsph.edu/research/black-lives-matter-protests-and-covid-19-cases-relationship-in-two-databases/
https://www.healthline.com/health-news/black-lives-matter-protests-didnt-contribute-to-covid19-surge
https://www.usatoday.com/story/news/factcheck/2020/09/17/fact-check-sturgis-rallys-covid-19-cases-misstated-online-post/3458606001/
Last edited by dean on Sun Feb 21, 2021 8:07 pm; edited 1 time in total
dean- Posts : 5607
Join date : 2008-01-01
 asymptomatic and friends vs family
asymptomatic and friends vs family
https://academic.oup.com/cid/advance-article/doi/10.1093/cid/ciab100/6131730
SARS-CoV-2 setting-specific transmission rates: a systematic review and meta-analysis
Transmission
Thompson et al. (Feb 9, 2021). SARS-CoV-2 Setting-Specific Transmission Rates: A Systematic Review and Meta-Analysis. Clinical Infectious Diseases. https://doi.org/10.1093/cid/ciab100
https://www.medrxiv.org/content/10.1101/2020.04.04.20053058v1
Indoor transmission of SARS-CoV-2
SARS-CoV-2 setting-specific transmission rates: a systematic review and meta-analysis
Transmission
• A systematic review and meta-analysis indicated that the highest SARS-CoV-2 transmission rates were within households, with a pooled secondary attack rate (SAR) of 21%. SARs were significantly higher when the duration of household exposure was longer than 5 days. SARs for contacts with family and friends were higher than those for low-risk casual contacts (6% vs. 1%). Estimates of SAR for asymptomatic index cases were about seven times lower than those for symptomatic index cases. There was some evidence for reduced transmission potential both from and to individuals under 20 years of age in the household context, but there were limited data to examine transmission in other settings like schools and workplaces.
Thompson et al. (Feb 9, 2021). SARS-CoV-2 Setting-Specific Transmission Rates: A Systematic Review and Meta-Analysis. Clinical Infectious Diseases. https://doi.org/10.1093/cid/ciab100
https://www.medrxiv.org/content/10.1101/2020.04.04.20053058v1
Indoor transmission of SARS-CoV-2
Abstract
Background By early April 2020, the COVID-19 pandemic had infected nearly one million people and had spread to nearly all countries worldwide. It is essential to understand where and how SARS-CoV-2 is transmitted.
Methods Case reports were extracted from the local Municipal Health Commissions of 320 prefectural cities (municipalities) in China, not including Hubei province, between 4 January and 11 February 2020. We identified all outbreaks involving three or more cases and reviewed the major characteristics of the enclosed spaces in which the outbreaks were reported and associated indoor environmental issues.
Results Three hundred and eighteen outbreaks with three or more cases were identified, involving 1245 confirmed cases in 120 prefectural cities. We divided the venues in which the outbreaks occurred into six categories: homes, transport, food, entertainment, shopping, and miscellaneous. Among the identified outbreaks, 53·8% involved three cases, 26·4% involved four cases, and only 1·6% involved ten or more cases. Home outbreaks were the dominant category (254 of 318 outbreaks; 79·9%), followed by transport (108; 34·0%; note that many outbreaks involved more than one venue category). Most home outbreaks involved three to five cases. We identified only a single outbreak in an outdoor environment, which involved two cases.
Conclusions All identified outbreaks of three or more cases occurred in an indoor environment, which confirms that sharing indoor space is a major SARS-CoV-2 infection risk.
Last edited by dean on Sun Feb 21, 2021 8:08 pm; edited 1 time in total
dean- Posts : 5607
Join date : 2008-01-01
 Re: I do not believe it is airborn it is touch
Re: I do not believe it is airborn it is touch
i believe this site is way wrong in its analysis. But include it because they may have some good links.
I again believe a mask of any kind stops you from touching your mucous areas of your face the 10 times an hour you touch. That is what a mask does for you in a high risk area/situation.
https://swprs.org/face-masks-evidence/?fbclid=IwAR1-LU8ojxGsKurthSr-oIyN1yl1rVmTMR2wP9rFuKjIFTTDpOOg-gU8R2A
Are Face Masks Effective? The Evidence.
I again believe a mask of any kind stops you from touching your mucous areas of your face the 10 times an hour you touch. That is what a mask does for you in a high risk area/situation.
https://swprs.org/face-masks-evidence/?fbclid=IwAR1-LU8ojxGsKurthSr-oIyN1yl1rVmTMR2wP9rFuKjIFTTDpOOg-gU8R2A
Are Face Masks Effective? The Evidence.
dean- Posts : 5607
Join date : 2008-01-01
 Re: I do not believe it is airborn it is touch
Re: I do not believe it is airborn it is touch
this one found there was no correlation to being safer wearing a mask. ya with caveats.
https://www.thelancet.com/journals/laninf/article/PIIS1473-3099(20)30985-3/fulltext?fbclid=IwAR1cuMiAbdbZyrUQ1CIfqhECI_GZy4QcG1gTFuW68bmcAydgONT3MBd4O3k
Transmission of COVID-19 in 282 clusters in Catalonia, Spain: a cohort study
the next one is deceptive. the farther you physically distance the less likely you tough items in common.
https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(20)31142-9/fulltext?fbclid=IwAR0srlgvkPDxRBd93mg25lCFkMPQwPL8jWva4Y3-4ToZGgXJkwkraJqyUu4
Physical distancing, face masks, and eye protection to prevent person-to-person transmission of SARS-CoV-2 and COVID-19: a systematic review and meta-analysis
[quote]
https://www.thelancet.com/journals/laninf/article/PIIS1473-3099(20)30985-3/fulltext?fbclid=IwAR1cuMiAbdbZyrUQ1CIfqhECI_GZy4QcG1gTFuW68bmcAydgONT3MBd4O3k
Transmission of COVID-19 in 282 clusters in Catalonia, Spain: a cohort study
Introduction
According to current evidence, COVID-19 is primarily transmitted from person to person through respiratory droplets, as well as indirect contact through transfer of the virus from contaminated fomites to the mouth, nose, or eyes.1, 2 As with most respiratory viral infections, some transmission through smaller aerosols is likely to occur, but their relative contribution compared with droplets remains unclear. Several outbreak investigation reports have shown that COVID-19 transmission can be particularly effective in confined indoor spaces such as workplaces, including factories, churches, restaurants, shopping centres, and health-care settings.3, 4, 5, 6 In Spain and many other countries, health-care workers have had a high rate of COVID-19 infection.7
the next one is deceptive. the farther you physically distance the less likely you tough items in common.
https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(20)31142-9/fulltext?fbclid=IwAR0srlgvkPDxRBd93mg25lCFkMPQwPL8jWva4Y3-4ToZGgXJkwkraJqyUu4
Physical distancing, face masks, and eye protection to prevent person-to-person transmission of SARS-CoV-2 and COVID-19: a systematic review and meta-analysis
[quote]
dean- Posts : 5607
Join date : 2008-01-01
 all super sreader were indoors as defined by 3 cases from on
all super sreader were indoors as defined by 3 cases from on
https://onlinelibrary.wiley.com/doi/10.1111/ina.12766
https://www.medrxiv.org/content/10.1101/2020.04.04.20053058v1
Indoor transmission of SARS-CoV-2
It is essential to understand where and how severe acute respiratory syndrome coronavirus 2 (SARS‐CoV‐2) is transmitted. Case reports were extracted from the local Municipal Health Commissions of 320 prefectural municipalities in China (not including Hubei Province). We identified all outbreaks involving three or more cases and reviewed the major characteristics of the enclosed spaces in which the outbreaks were reported and their associated indoor environmental aspects. Three hundred and eighteen outbreaks with three or more cases were identified, comprising a total of 1245 confirmed cases in 120 prefectural cities. Among the identified outbreaks, 53.8% involved three cases, 26.4% involved four cases, and only 1.6% involved ten or more cases. Home‐based outbreaks were the dominant category (254 of 318 outbreaks; 79.9%), followed by transport‐based outbreaks (108; 34.0%), and many outbreaks occurred in more than one category of venue. All identified outbreaks of three or more cases occurred in indoor environments, which confirm that sharing indoor spaces with one or more infected persons is a major SARS‐CoV‐2 infection risk.
https://www.medrxiv.org/content/10.1101/2020.04.04.20053058v1
Indoor transmission of SARS-CoV-2
Background By early April 2020, the COVID-19 pandemic had infected nearly one million people and had spread to nearly all countries worldwide. It is essential to understand where and how SARS-CoV-2 is transmitted.
Methods Case reports were extracted from the local Municipal Health Commissions of 320 prefectural cities (municipalities) in China, not including Hubei province, between 4 January and 11 February 2020. We identified all outbreaks involving three or more cases and reviewed the major characteristics of the enclosed spaces in which the outbreaks were reported and associated indoor environmental issues.
Results Three hundred and eighteen outbreaks with three or more cases were identified, involving 1245 confirmed cases in 120 prefectural cities. We divided the venues in which the outbreaks occurred into six categories: homes, transport, food, entertainment, shopping, and miscellaneous. Among the identified outbreaks, 53·8% involved three cases, 26·4% involved four cases, and only 1·6% involved ten or more cases. Home outbreaks were the dominant category (254 of 318 outbreaks; 79·9%), followed by transport (108; 34·0%; note that many outbreaks involved more than one venue category). Most home outbreaks involved three to five cases. We identified only a single outbreak in an outdoor environment, which involved two cases.
Conclusions All identified outbreaks of three or more cases occurred in an indoor environment, which confirms that sharing indoor space is a major SARS-CoV-2 infection risk.
Last edited by dean on Sun Feb 21, 2021 8:10 pm; edited 2 times in total
dean- Posts : 5607
Join date : 2008-01-01
 outdoor vs indoor
outdoor vs indoor
https://www.sciencedirect.com/science/article/pii/S0013935120315000?via%3Dihub
On the concentration of SARS-CoV-2 in outdoor air and the interaction with pre-existing atmospheric particles
On the concentration of SARS-CoV-2 in outdoor air and the interaction with pre-existing atmospheric particles
dean- Posts : 5607
Join date : 2008-01-01
 Handwashing and risk of respiratory infections: a quantitati
Handwashing and risk of respiratory infections: a quantitati
https://www.cdc.gov/handwashing/why-handwashing.html#five
Show Me the Science - Why Wash Your Hands?
https://pubmed.ncbi.nlm.nih.gov/16553905/
Handwashing and risk of respiratory infections: a quantitative systematic review
https://www.cochrane.org/CD006207/ARI_do-physical-measures-such-hand-washing-or-wearing-masks-stop-or-slow-down-spread-respiratory-viruses
Do physical measures such as hand-washing or wearing masks stop or slow down the spread of respiratory viruses?
http://discover.uw.edu/x0A003080vL0x8Q08yFimOX
https://www.cochranelibrary.com/cdsr/doi/10.1002/14651858.CD006207.pub5/full
Show Me the Science - Why Wash Your Hands?
Reduces respiratory illnesses, like colds, in the general population by 16-21% 3, 5
https://pubmed.ncbi.nlm.nih.gov/16553905/
Handwashing and risk of respiratory infections: a quantitative systematic review
Results: All eight eligible studies reported that handwashing lowered risks of respiratory infection, with risk reductions ranging from 6% to 44% [pooled value 24% (95% CI 6-40%)]. Pooling the results of only the seven homogenous studies gave a relative risk of 1.19 (95% CI 1.12%-1.26%), implying that hand cleansing can cut the risk of respiratory infection by 16% (95% CI 11-21%).
Conclusions: Handwashing is associated with lowered respiratory infection. However, studies were of poor quality, none related to developing countries, and only one to severe disease. Rigorous trials of the impact of handwashing on acute respiratory tract infection morbidity and mortality are urgently needed, especially in developing countries.
https://www.cochrane.org/CD006207/ARI_do-physical-measures-such-hand-washing-or-wearing-masks-stop-or-slow-down-spread-respiratory-viruses
Do physical measures such as hand-washing or wearing masks stop or slow down the spread of respiratory viruses?
Hand hygiene
Following a hand hygiene programme may reduce the number of people who catch a respiratory or flu-like illness, or have confirmed flu, compared with people not following such a programme (16 studies; 61,372 people). Few studies measured unwanted effects; skin irritation in people using hand sanitiser was mentioned.
http://discover.uw.edu/x0A003080vL0x8Q08yFimOX
• A meta-analysis with 67 pre-COVID-19 trials reported no significant reduction in respiratory viral infection with the use of medical/surgical masks during influenza season (9 trials; 3507 participants), and no clear differences between the use of medical/surgical masks versus N95/P2 respirators in healthcare workers (5 trials; 8407 participants). Hand hygiene was associated with an 11% relative reduction of respiratory illness (7 trials; 44,129 participants) but with low-certainty evidence and high heterogeneity.
https://www.cochranelibrary.com/cdsr/doi/10.1002/14651858.CD006207.pub5/full
dean- Posts : 5607
Join date : 2008-01-01
 Re: I do not believe it is airborn it is touch
Re: I do not believe it is airborn it is touch
Assessing Mandatory Stay‐at‐Home and Business Closure Effects on the Spread of COVID‐19
https://onlinelibrary.wiley.com/doi/10.1111/eci.13484
https://onlinelibrary.wiley.com/doi/10.1111/eci.13484
dean- Posts : 5607
Join date : 2008-01-01
 Re: I do not believe it is airborn it is touch
Re: I do not believe it is airborn it is touch
https://wwwnc.cdc.gov/eid/article/27/3/20-4714_article
Abstract
Since the first wave of coronavirus disease in March 2020, citizens and permanent residents returning to New Zealand have been required to undergo managed isolation and quarantine (MIQ) for 14 days and mandatory testing for severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). As of October 20, 2020, of 62,698 arrivals, testing of persons in MIQ had identified 215 cases of SARS-CoV-2 infection. Among 86 passengers on a flight from Dubai, United Arab Emirates, that arrived in New Zealand on September 29, test results were positive for 7 persons in MIQ. These passengers originated from 5 different countries before a layover in Dubai; 5 had negative predeparture SARS-CoV-2 test results. To assess possible points of infection, we analyzed information about their journeys, disease progression, and virus genomic data. All 7 SARS-CoV-2 genomes were genetically identical, except for a single mutation in 1 sample. Despite predeparture testing, multiple instances of in-flight SARS-CoV-2 transmission are likely.
Abstract
Since the first wave of coronavirus disease in March 2020, citizens and permanent residents returning to New Zealand have been required to undergo managed isolation and quarantine (MIQ) for 14 days and mandatory testing for severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). As of October 20, 2020, of 62,698 arrivals, testing of persons in MIQ had identified 215 cases of SARS-CoV-2 infection. Among 86 passengers on a flight from Dubai, United Arab Emirates, that arrived in New Zealand on September 29, test results were positive for 7 persons in MIQ. These passengers originated from 5 different countries before a layover in Dubai; 5 had negative predeparture SARS-CoV-2 test results. To assess possible points of infection, we analyzed information about their journeys, disease progression, and virus genomic data. All 7 SARS-CoV-2 genomes were genetically identical, except for a single mutation in 1 sample. Despite predeparture testing, multiple instances of in-flight SARS-CoV-2 transmission are likely.
dean- Posts : 5607
Join date : 2008-01-01
 Re: I do not believe it is airborn it is touch
Re: I do not believe it is airborn it is touch
well here they state that cloth masks and surgical are not effective at airborne... thats why we know it is contact, again japan high use of cloth and 1/50th of the rates of the usa. It is a contact barrier wearing a mask... again proven they do not work for airborne particles, so the default is they are effective so they are effective at stopping you from touching your face directly specially the mucous areas in high risk locations. Wear a mask... but not for airborne protection.
As I have noted that in the summer massive protests people were not socially distanced and yelling at the top of their lungs and to date no super spreading events on these 100s of massive protests. Where right now states are having massive record numbers of cases and deaths and no protests. Sturges was a massive gathering, and it is referred to as a super spreader event, the problem at sturges was the bars and concerts with drinking. These bars are overwhelmed with customers in a short period and no way to maintain the needed levels of cleaning and employee hygiene as mistakes happen. While it was noted as a super spreader event the numbers were not that massive because it was mainly outdoors. To me outdoors means not mainly items where there is mutual contact where people are offguard. examples, People would be on-guard when using a washroom. People would not be onguard touching a chair to sit in it or move it slightly.
Can face masks offer protection from airborne sneeze and cough droplets in close-up, face-to-face human interactions?—A quantitative study featured
Akhtar et al. (Dec 22, 2020). Can Face Masks Offer Protection from Airborne Sneeze and Cough Droplets in Close-up, Face-to-Face Human Interactions?—A Quantitative Study. Physics of Fluids. https://doi.org/10.1063/5.0035072
https://aip.scitation.org/doi/10.1063/5.0035072
As I have noted that in the summer massive protests people were not socially distanced and yelling at the top of their lungs and to date no super spreading events on these 100s of massive protests. Where right now states are having massive record numbers of cases and deaths and no protests. Sturges was a massive gathering, and it is referred to as a super spreader event, the problem at sturges was the bars and concerts with drinking. These bars are overwhelmed with customers in a short period and no way to maintain the needed levels of cleaning and employee hygiene as mistakes happen. While it was noted as a super spreader event the numbers were not that massive because it was mainly outdoors. To me outdoors means not mainly items where there is mutual contact where people are offguard. examples, People would be on-guard when using a washroom. People would not be onguard touching a chair to sit in it or move it slightly.
Can face masks offer protection from airborne sneeze and cough droplets in close-up, face-to-face human interactions?—A quantitative study featured
• With the exception of N95 masks, face coverings would not offer complete protection for a susceptible person exposed to coughing or sneezing of an infected person within 6 feet according to droplet flow visualization experiments. While no potentially virus-carrying particles were observed to leak through N95 masks when worn as protection, enough particles were found to leak through other face coverings, such as surgical and double-layer cloth masks, to expose the wearer to a sufficiently infectious dose.
Akhtar et al. (Dec 22, 2020). Can Face Masks Offer Protection from Airborne Sneeze and Cough Droplets in Close-up, Face-to-Face Human Interactions?—A Quantitative Study. Physics of Fluids. https://doi.org/10.1063/5.0035072
https://aip.scitation.org/doi/10.1063/5.0035072
dean- Posts : 5607
Join date : 2008-01-01
 Re: I do not believe it is airborn it is touch
Re: I do not believe it is airborn it is touch
https://www.cntraveler.com/story/a-guide-to-kissing-etiquette-around-the-world
A Guide to Kissing Etiquette Around the World
A Guide to Kissing Etiquette Around the World
The Cheat Sheet
Not only is it worthwhile to know where you might have to turn a cheek, but it’s helpful to know just how many kisses to expect. In France alone, the count varies dramatically by region, according to a 2014 web survey of more than 100,000 citizens: Parisians consider two kisses the norm, while three is standard in Provence, and four throughout the Loire Valley. Here’s the common count for a sampling of other countries:
One Kiss: Colombia, Argentina, Chile, Peru, the Philippines
Two Kisses: Spain, Italy, Greece, Germany, Hungary, Romania, Croatia, Bosnia, Brazil (though, like France, the number can differ by region), and some Middle Eastern countries (though not between opposite sexes)
Three Kisses: Belgium, Slovenia, Macedonia, Montenegro, Serbia, the Netherlands, Switzerland, Egypt, and Russia (where it’s accompanied by a bear hug)
dean- Posts : 5607
Join date : 2008-01-01
 Re: I do not believe it is airborn it is touch
Re: I do not believe it is airborn it is touch
https://jamanetwork.com/journals/jamanetworkopen/fullarticle/2774463
December 23, 2020
Assessment of Air Contamination by SARS-CoV-2 in Hospital
[SettingsQuestion What is the level of air contamination from severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) in different hospital areas, and what factors are associated with contamination?
Findings In this systematic review of 24 studies, 17% of air sampled from close patient environments was positive for SARS-CoV-2 RNA, with viability of the virus found in 9% of cultures.
Meaning In this study, air both close to and distant from patients with coronavirus disease 2019 was frequently contaminated with SARS-CoV-2 RNA; however, few of these samples contained viable viruses.
December 23, 2020
Assessment of Air Contamination by SARS-CoV-2 in Hospital
[SettingsQuestion What is the level of air contamination from severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) in different hospital areas, and what factors are associated with contamination?
Findings In this systematic review of 24 studies, 17% of air sampled from close patient environments was positive for SARS-CoV-2 RNA, with viability of the virus found in 9% of cultures.
Meaning In this study, air both close to and distant from patients with coronavirus disease 2019 was frequently contaminated with SARS-CoV-2 RNA; however, few of these samples contained viable viruses.
dean- Posts : 5607
Join date : 2008-01-01
 Re: I do not believe it is airborn it is touch
Re: I do not believe it is airborn it is touch
here is a write up, they found basically no proof at all being airborne. They even used the stupid one like the choir which no one discussed the chairs they moved or the brakroom where thy ate and could have passed around drinks or food. Or touching the doorknob to enter ar use the bathroom or sink.
https://depts.washington.edu/pandemicalliance/wordpress/wp-content/uploads/2020/12/Summary-Ventilation_2020_12_21-003.pdf?mkt_tok=eyJpIjoiTURObE9EVmxNR00wTjJNMCIsInQiOiJxNFFKbjhXWXl6Q0pDZUJSclBWNVl0dndManBWVThVV0J2Y2FQT2c5WXk1WU1oWmNTSDdzQVFkZUNYYVwvZzJHY3dEUmJxY0NDRmp4MjZFOUR3SkRpRmVuTWFCNVluNFgwMUpLczNNU0RJcjhrdGxSMVZkNUpQbHNFblRTVWhWcXQifQ%3D%3D
Summary of Evidence Related to Indoor Ventilation to Reduce SARS-CoV-2 Transmission
https://depts.washington.edu/pandemicalliance/wordpress/wp-content/uploads/2020/12/Summary-Ventilation_2020_12_21-003.pdf?mkt_tok=eyJpIjoiTURObE9EVmxNR00wTjJNMCIsInQiOiJxNFFKbjhXWXl6Q0pDZUJSclBWNVl0dndManBWVThVV0J2Y2FQT2c5WXk1WU1oWmNTSDdzQVFkZUNYYVwvZzJHY3dEUmJxY0NDRmp4MjZFOUR3SkRpRmVuTWFCNVluNFgwMUpLczNNU0RJcjhrdGxSMVZkNUpQbHNFblRTVWhWcXQifQ%3D%3D
Summary of Evidence Related to Indoor Ventilation to Reduce SARS-CoV-2 Transmission
Summary of Evidence Related to Indoor Ventilation to Reduce SARS-CoV-2 Transmission
December 21, 2020
COVID-19 Literature Report Team:
Lorenzo Tolentino MPH , Jennifer M. Ross MD MPH, Jessie Seiler MPH,
Wenwen Jiang MPH, Sherrilynne Fuller PhD FACMI, Dylan Green MPH, Diana M. Tordoff MPH, Diana
Louden MLib, Alison Drake PhD MPH, Will Hahn MD, and Brandon L. Guthrie PhD
Mitigation of SARS-CoV-2 transmission in indoor spaces is crucial, especially during the winter season
when activities are mostly held in enclosed indoor environments. Understanding SARS-CoV-2 transmission
mechanisms relating to ventilation of indoor air and what evidence-based environmental measures are
available will be key to infection control. This document is a brief summary of published evidence on
SARS-CoV-2 transmission mechanisms that relate to ventilation of indoor spaces and ventilation
standards/best practices for minimizing spread. References are mainly drawn from the COVID-19
Literature Report (Lit Rep) team database and guidelines published by the CDC. References that appeared
in the daily Lit Rep are marked with an asterisk*, and the summary is shown in the annotated
bibliography below.
Executive Summary of Ventilation and SARS-CoV-2
• Most evidence suggests SARS-CoV-2 is largely transmitted through close contact and larger
respiratory droplets. A small number of studies have isolated viable virus from air samples in
lab and clinical settings and SARS-CoV-2 airborne transmission beyond 6 feet has only been
observed in poorly ventilated and crowded indoor spaces.
• While SARS-CoV-2 RNA has been detected in heating, ventilation, and air conditioning (HVAC)
systems, viable virus was not isolated. There has been no documented evidence of SARS-CoV2 transmission occurring through HVAC systems.
• Ventilation standards/best practices to reduce risk of SARS-CoV-2 transmission primarily
include methods to decrease concentrations of aerosols that may carry infectious virus either
through filtration of indoor air or circulation of cleaner air from outside.
• Ventilation standards/best practices alone are not enough to mitigate SARS-CoV-2
transmission. They should only be implemented in conjunction with infection control
measures that more directly address SARS-CoV-2 primary modes of transmission, such as
reducing building occupancy to facilitate physical distancing, mask wearing, surface
disinfection, and handwashing.
SARS-CoV-2 Transmission related to Ventilation
Note: Some of the evidence covered here can also be found in the CDC brief on SARS-CoV-2 and Potential
Airborne Transmission.
Aerosol Transmission
• Particles ejected when an infectious person sneezes, coughs, sings, or breathes form a spectrum
of respiratory droplets and aerosols.
Updated 12/21/2020
o Respiratory droplets are large droplets (>5 μm in diameter) that settle more quickly on
surrounding surfaces. They are responsible for droplet transmission, which occurs when
a person in close contact (within about 6 feet) inhales these droplets.
o Aerosols (<5 μm in diameter) are smaller, lighter particles which can remain airborne for
much longer and can be carried farther by airflow and wind currents. They are responsible
for airborne transmission, which occurs when a person inhales these particles.
• The SARS-CoV-2 virus, which is around 0.1 μm, generally does not travel through the air by itself.
Potentially infectious virus (based on replication in cell culture) has been isolated from air samples
as well as from surfaces on which respiratory droplets have deposited,
1,2* indicating that particles
of varying size can be laden with infectious virus.
• While other coronaviruses are more likely to be present in aerosols than in larger respiratory
droplets,
3 the exact distribution of the SARS-CoV-2 across the range of different-sized particles is
unknown.
No substantial evidence on classic long-range airborne transmission
• Currently, there is no substantial evidence that SARS-CoV-2 can be transmitted efficiently over
long distances through airborne transmission like other pathogens such as TB, measles, or
varicella (chickenpox).
4
• Though aerosolized SARS-CoV-2 virus has been shown to be stable in aerosols for 3-16 hours in
laboratory settings,1,5 real-world factors such as temperature and relative humidity affect the
stability of the virus, while ventilation and exhaled viral load affect the concentration necessary
to infect others.
• Given the significant proportion of infections caused by persons with asymptomatic SARS-CoV-2
infection, it is estimated that global spread would have occurred much more rapidly if SARS-CoV2 spread primarily through airborne transmission.
6
Evidence of short-range airborne transmission in certain conditions
While uncommon, several instances of “short-range” airborne transmission beyond what could be
attributed to droplet transmission alone have been documented. These events are associated with
enclosed, indoor settings with poor or improper ventilation, prolonged exposure to infectious persons,
and activities that increase the rate of droplet and aerosol generation:
• An outbreak occurred in a restaurant in which directional airflow from an air conditioner is
suspected to have transmitted infected aerosols from the table of the index patient to adjacent
tables.
7
*
• An outbreak during a 2.5-hour choir practice with an attack rate of 53-87% occurred, with indoor
transmission likely augmented by singing.
8
• An outbreak involving two 50-minute rides inside a bus with recirculating air occurred, with
secondary individuals sitting closer to the index case being no more likely to get infected than
those sitting farther, indicating an extended range of transmission.9
*
• In an outbreak in 1 out of 7 wards of a nursing home during a period of low community incidence
occurred, the ward experiencing the outbreak had recently installed demand-controlled
ventilation that only circulated outside air based on indoor CO2 levels.
10*
• A cluster of cases were associated with a shopping mall, where possible virus aerosolization
occurring in confined spaces such as elevators and restrooms and contributed to indirect
transmission.
11
Updated 12/21/2020
• A cluster of cases associated with a squash court occurred, with individuals who played in the
same squash hall as the index case at least 45 minutes later were infected, possibly from
aerosols.
12
• An outbreak at a nightclub occurred in which infected staff likely caused multiple infections across
three different events.
13
• An outbreak of 112 cases occurred in 12 sports facilities over 24 days, where asymptomatic and
pre-symptomatic instructors taught fitness dance classes to 5–22 students in a room
approximately 60 m2 for 50 minutes of intense exercise.
14
Indoor Transmission through HVAC systems
We found no reported evidence of SARS-CoV-2 transmission occurring through heating, ventilation, and
air conditioning (HVAC) systems. SARS-CoV-2 RNA has been detected in multiple parts of HVAC systems,
though viable virus was not isolated. However, a potential limitation of available evidence is that the
sampling timeframe may not have captured the virus when it was infectious.
• Positive samples (swab and cell media) for SARS-CoV-2 RNA were found in the HVAC system of
COVID-19 wards and in the central HVAC system, which was located 5 floors above. Viral culture
was unable to detect viable virus in samples.
15*
• Tests for SARS-CoV-2 RNA were negative for swabs and air samples collected from the Diamond
Princess cruise ship in cabins with no COVID-19 cases, but that shared air circulation with COVID19 cabins via the HVAC system.16*
• Presence of SAR-CoV-2 RNA was detected in 25% of samples collected in 9 locations of the HVAC
system of a university hospital in Oregon. These samples were not evaluated for viral
infectiousness.
17
Ventilation Standards/Best Practices
Note: Some of the guidelines covered here can also be found in the Washington Department of Health
ventilation guidance and CDC ventilation guidance.
Given that SARS-CoV-2 is largely transmitted through close contact and larger respiratory droplets,
precautions are recommended and the addition of ventilation measures should be considered a
component in a layered approach. Ventilation measures should not be designed to completely substitute
other measures such as PPE, mask use, surface disinfection, and personal hygiene. Implementation of
some ventilation measures outlined here require technical expertise, and consultation with an HVAC
specialist or professional engineer is recommended.
Ventilation measures reduce the risk of SARS-CoV-2 transmission by diluting the concentration of
infectious aerosols in the environment. This is primarily achieved by filtration of indoor air or circulation
of cleaner air from the outside, either through 1) a central HVAC system, or 2) non-HVAC measures.
Ventilation measures affect the air exchange rate per hour (ACH), which is defined as the number of times
the air occupying the volume of a given space is exchanged with cleaner air.
HVAC Measures
• The CDC recommends installing filters in the HVAC system with the highest performance that
the system can handle. The American Society of Heating, Refrigerating and Air-Conditioning
Engineers (ASHRAE) recommends installing filters with at least Minimum Efficiency Reporting
Updated 12/21/2020
Value (MERV) of 13, provided there is no substantial impact on HVAC performance or occupant
comfort.
o MERV values range from 1 to 16, with higher values corresponding to better efficiency.
MERV 13 filters are at least 50% efficient at capturing particles in the 0.3 µm to 1.0 µm
size range and 85% efficient at capturing particles in the 1 µm to 3 µm size range (more
information on MERV standards can be found here.
o Higher MERV values can cause a drop in air pressure as more air is filtered, but provide
cleaner air with which to exchange the existing air in an enclosed space.
• Turn off demand-controlled ventilation, which automatically circulates outside air based on
temperature, humidity, or CO2 concentrations, to avoid build-up of indoor air
• Allow for HVAC systems to circulate outside air. Run HVAC systems on maximum to flush indoor
air 2 hours before and after occupancy.
o The CDC has guidelines for how long a system performing at certain ACH must be run in
order to remove the recommended 99% of airborne contaminants.
• Open outdoor air dampers to reduce or eliminate HVAC indoor air recirculation (this may be
difficult in hot or humid weather)
• Maintain relative humidity at 40-60% and temperature within 68-78F (ASHRAE guidance for
residential)
o Ecological studies have found higher transmission rates in geographical regions with
colder and dryer air; however, there is considerable potential for confounding in these
comparisons, and the role of temperature and humidity in SARS-CoV-2 infectiousness is
not clearly established.
18
o Surface stability of SARS-CoV-2 has been found to decrease with increasing temperature
and humidity.
19*
• Ensure that minimum rates for outdoor air circulation are met or exceeded.
o These minimum rates not only depend upon the room size, but also the number of
occupants, typical activities conducted within the room, and other environmental
factors. In general, doubling the occupancy will double the minimum required rate. For
more comprehensive standards and calculations for a wide variety of settings, see
Equation 6-1 and Table 6-1 of ASHRAE 62.1 (2019)
Non-HVAC Measures
These measures are best used to augment HVAC measures and are best implemented in settings with
limited or nonexistent HVAC systems.
• Place portable High Efficiency Particulate (HEPA) filter-equipped systems in critical areas.
o High Efficiency Particulate (HEPA) filters are at least 99.97% efficient in capturing
particles 0.3 μm in size and are even more efficient in capturing particles that are both
smaller and larger.
o As particles increase in size from 0.3 μm, they are more likely to be strained or blocked
since they cannot pass through the tightly woven fiber mesh of the filter. As particles
decrease in size from 0.3μm, their movement is increasingly dictated by random
diffusional collisions with other molecules rather than the airflow, and thus have
increasing probability to collide with the large combined surface area of every fiber in
the filter (see page 3 and page 7 of this NASA report for a more detailed explanation).
Updated 12/21/2020
o Portable HEPA-equipped systems have a Clean Air Delivery Rate (CADR) measured in
cubic feet per minute (cfm), which dictates how quickly they can remove particles in the
air of a room of a given size. Bigger rooms require systems with higher CADR.
Table: Portable Air Cleaner Size for Particle Removal (EPA)
Room area (ft2) 100 200 300 400 500 600
Minimum CADR (cfm) 65 130 195 260 325 390
For estimation purposes in a home setting. CADRs are calculated based on an 8 ft.
ceiling and an ACH of 4.875.
o A study (pre-print, not peer reviewed) found that HEPA filters installed in a poorlyventilated classroom setting with a combined ACH of 5.7 could reduce the inhaled viral
dose from a super-spreader in a room by a factor of 6.20*
• Open windows and doors to outside air. Use caution if outdoor air quality is poorer or not ideal
for occupant comfort (e.g. high pollution, colder outdoor weather).
• Use indoor fans to facilitate airflow following a clean-to-less-clean air pattern and blowing away
from people
o Place fans near windows or doors to blow out indoor air
o Reverse direction of ceiling fans to pull air up
• Reduce occupancy as much as possible to allow for physical distancing, and avoid occupant
activities that cause higher rates of emitting respiratory droplets and aerosols (e.g., singing,
shouting, cheering)
• Use faces coverings
o Face masks or other face coverings function as filters that are closest to the source of
infectious aerosols and can drastically reduce the concentration of viral particles in
indoor environments.
o Hospital rooms with unmasked COVID-19 patients, despite extensive ventilation
measures, were found to contain RNA-positive surface samples21 and air samples with
viable virus.2
*
o Air samples collected in indoor spaces (hotel room, car) where an individual who had
either confirmed influenza or suspected COVID-19 wore a cotton/surgical mask showed
a substantial decrease in aerosol concentration.
22*
o A modeling study exploring risk of transmission from super-spreaders in various indoor
settings (e.g. schools, offices) found that active ventilation combined with mask use
outperformed portable HEPA filtration with up to 9 ACH in all scenarios.
23
Ventilation Considerations for Special Settings: Schools
• HVAC and non-HVAC measures summarized here can be applied to a wide variety of contexts.
For example, in schools, the CDC ventilation guidance recommends increasing outdoor
ventilation by opening windows and using fans, improving central air filtration, and using
portable HEPA filtration systems in high-risk areas such as nurses offices.
• Maintain temperature and relative humidity at 72°F and 40-50% (ASHRAE winter classroom
guidelines).
Updated 12/21/2020
Other Measures
• Germicidal Ultraviolet Irradiation (GUVI)
o GUVI, which employs UV-C to inactivate fungal, bacterial, and viral pathogens, can be
installed in ducts or as ceiling fixtures to disinfect indoor air (see ASHRAE guidelines)
o GUVI can be costly (can be upwards of $1,500) and potentially harmful to occupants,
thus they are typically only used in high-risk settings such as TB wards.
o A modeling study estimates that installation of safer far-UVC in populated rooms could
increase SARS-CoV-2 disinfection rates by 50-85%.
dean- Posts : 5607
Join date : 2008-01-01
 Re: I do not believe it is airborn it is touch
Re: I do not believe it is airborn it is touch
https://www.atsjournals.org/doi/pdf/10.1164/rccm.202006-2136LE
SARS-CoV-2 Detected on Environmental Fomites for both Asymptomatic and
Symptomatic COVID-19 Patients
SARS-CoV-2 Detected on Environmental Fomites for both Asymptomatic and
Symptomatic COVID-19 Patients
• SARS-CoV-2 RNA was detected on surfaces in the rooms of both symptomatic and asymptomatic SARS-CoV-2 infected patients in a hospital in Shenzen, China. Among asymptomatic patients, samples from squat toilets showed the highest positivity rate, followed by samples related to mouth or nose contact (e.g. water cup, straw), and then samples from inside masks worn by the patients. A significantly higher proportion of samples were positive from the rooms of patients with higher viral load among patients who were symptomatic, while a similar but nonsignificant relationship was observed among patients who were asymptomatic. All samples collected from surfaces following disinfection with alcohol or chlorine-containing solutions were negative in both symptomatic and asymptomatic groups.
Yang et al. (Dec 16, 2020). SARS-CoV-2 Detected on Environmental Fomites for Both Asymptomatic and Symptomatic COVID-19 Patients. American Journal of Respiratory and Critical Care Medicine. https://doi.org/10.1164/rccm.202006-2136LE
dean- Posts : 5607
Join date : 2008-01-01
 food plants door handles
food plants door handles
you do not breath on a door handle.
not peer reviewed.
https://www.medrxiv.org/content/10.1101/2020.12.10.20247171v1
Environmental monitoring shows SARS-CoV-2 contamination of surfaces in food plants
Ming et al. (Dec 11, 2020). Environmental Monitoring Shows SARS-CoV-2 Contamination of Surfaces in Food Plants. Pre-print downloaded Dec 14 from https://doi.org/10.1101/2020.12.10.20247171
not peer reviewed.
https://www.medrxiv.org/content/10.1101/2020.12.10.20247171v1
Environmental monitoring shows SARS-CoV-2 contamination of surfaces in food plants
• [Preprint, not peer-reviewed] In a study collecting 22,643 surface samples from 116 food processing facilities in the US from Mar 17 to Sep 3, 2020, 1.2% of the total samples tested positive for SARS-CoV-2 by PCR. 62 (53%) facilities had at least one sample positive for SARS-CoV-2. Among the positive samples, 33% were found on doorknobs/handles. The authors suggest that environmental surveillance for SARS-CoV-2 may aid in identifying workplaces with SARS-CoV-2 transmission.
Ming et al. (Dec 11, 2020). Environmental Monitoring Shows SARS-CoV-2 Contamination of Surfaces in Food Plants. Pre-print downloaded Dec 14 from https://doi.org/10.1101/2020.12.10.20247171
Highlights
Environmental contamination by SARS-CoV-2 virus was detected in food plants
Out of 22,643 environmental swabs, 278 (1.23%) were positive for SARS-CoV-2
Frequently touched surfaces had the most contamination
Surface testing for SARS-CoV-2 may indicate presence of asymptomatic carriers
Last edited by dean on Sun Feb 21, 2021 8:58 pm; edited 1 time in total
dean- Posts : 5607
Join date : 2008-01-01
 Re: I do not believe it is airborn it is touch
Re: I do not believe it is airborn it is touch
https://pubs.acs.org/doi/10.1021/acs.est.0c05651
A Systematic Review of Surface Contamination, Stability, and Disinfection Data on SARS-CoV-2 (Through July 10, 2020)
https://www.medrxiv.org/content/10.1101/2020.11.20.20220749v1
Community Transmission of SARS-CoV-2 by Fomites: Risks and Risk Reduction Strategies
A Systematic Review of Surface Contamination, Stability, and Disinfection Data on SARS-CoV-2 (Through July 10, 2020)
We conducted a systematic review of hygiene intervention effectiveness against SARS-CoV-2, including developing inclusion criteria, conducting the search, selecting articles for inclusion, and summarizing included articles. Overall, 96 268 articles were screened and 78 articles met inclusion criteria with outcomes in surface contamination, stability, and disinfection. Surface contamination was assessed on 3343 surfaces using presence/absence methods. Laboratories had the highest percent positive surfaces (21%, n = 83), followed by patient-room healthcare facility surfaces (17%, n = 1170), non-COVID-patient-room healthcare facility surfaces (12%, n = 1429), and household surfaces (3%, n = 161). Surface stability was assessed using infectivity, SARS-CoV-2 survived on stainless steel, plastic, and nitrile for half-life 2.3–17.9 h. Half-life decreased with temperature and humidity increases, and was unvaried by surface type. Ten surface disinfection tests with SARS-CoV-2, and 15 tests with surrogates, indicated sunlight, ultraviolet light, ethanol, hydrogen peroxide, and hypochlorite attain 99.9% reduction. Overall there was (1) an inability to align SARS-CoV-2 contaminated surfaces with survivability data and effective surface disinfection methods for these surfaces; (2) a knowledge gap on fomite contribution to SARS-COV-2 transmission; (3) a need for testing method standardization to ensure data comparability; and (4) a need for research on hygiene interventions besides surfaces, particularly handwashing, to continue developing recommendations for interrupting SARS-CoV-2 transmission.
https://www.medrxiv.org/content/10.1101/2020.11.20.20220749v1
Community Transmission of SARS-CoV-2 by Fomites: Risks and Risk Reduction Strategies
SARS-CoV-2, the virus responsible for the COVID-19 pandemic, is perceived to be primarily transmitted via person-to-person contact, through droplets produced while talking, coughing, and sneezing. Transmission may also occur through other routes, including contaminated surfaces; nevertheless, the role that surfaces have on the spread of the disease remains contested. Here we use the Quantitative Microbial Risk Assessment framework to examine the risks of community transmission of SARS-CoV-2 through contaminated surfaces and to evaluate the effectiveness of hand and surface disinfection as potential interventions. The risks posed by contacting surfaces in communities are low (average of the median risks 1.6x10-4 - 5.6x10-9) for community infection prevalence rates ranging from 0.2-5%. Hand disinfection substantially reduces relative risks of transmission independently of the disease's prevalence and the frequency of contact, even with low (25% of people) or moderate (50% of people) compliance. In contrast, the effectiveness of surface disinfection is highly dependent on the prevalence and the frequency of contacts. The work supports the current perception that contaminated surfaces are not a primary mode of transmission of SARS-CoV-2 and affirms the benefits of making hand disinfectants widely available.
dean- Posts : 5607
Join date : 2008-01-01
 Re: I do not believe it is airborn it is touch
Re: I do not believe it is airborn it is touch
https://www.cochranelibrary.com/cdsr/doi/10.1002/14651858.CD006207.pub5/full
Physical interventions to interrupt or reduce the spread of respiratory viruses
Physical interventions to interrupt or reduce the spread of respiratory viruses
• A meta-analysis with 67 pre-COVID-19 trials reported no significant reduction in respiratory viral infection with the use of medical/surgical masks during influenza season (9 trials; 3507 participants), and no clear differences between the use of medical/surgical masks versus N95/P2 respirators in healthcare workers (5 trials; 8407 participants). Hand hygiene was associated with an 11% relative reduction of respiratory illness (7 trials; 44,129 participants) but with low-certainty evidence and high heterogeneity.
Jefferson et al. (Nov 20, 2020). Physical Interventions to Interrupt or Reduce the Spread of Respiratory Viruses. The Cochrane Database of Systematic Reviews. https://doi.org/10.1002/14651858.CD006207.pub5
dean- Posts : 5607
Join date : 2008-01-01
 Re: I do not believe it is airborn it is touch
Re: I do not believe it is airborn it is touch
https://www.acpjournals.org/doi/10.7326/M20-6817
Effectiveness of Adding a Mask Recommendation to Other Public Health Measures to Prevent SARS-CoV-2 Infection in Danish Mask Wearers
Effectiveness of Adding a Mask Recommendation to Other Public Health Measures to Prevent SARS-CoV-2 Infection in Danish Mask Wearers
Non-Pharmaceutical Interventions
• An individually randomized controlled trial in Denmark from April to May 2020 (n=4,862) found that among participants spending at least 3 hours outside of home per day without occupational mask use and already practicing physical distancing, the intervention to recommend wearing a surgical mask when outside of home did not significantly reduce SARS-CoV-2 infection among mask wearers (OR = 0.82, 95% CI 0.54-1.23). Infection occurred in 42 participants recommended to wear masks (1.8%), compared to 53 participants in the control arm (2.1%). Accounting for loss to follow-up (19%) and mask use non-adherence (7%) yielded similar results.
• Key study limitations include 46% who reported adherence to wearing the mask as recommended and 47% who reported wearing the mask predominantly as recommended. The authors note that study findings are in the context of implementation of other public health measures, including social distancing, limiting contacts, and restaurant closures – including part of the trial occurring during lockdown. [EDITORIAL NOTE: This trial evaluated only the outcome of infections among people instructed to wear a mask, and not the effect of wearing masks on decreasing transmission to other people.]
Bundgaard et al. (Nov 18, 2020). Effectiveness of Adding a Mask Recommendation to Other Public Health Measures to Prevent SARS-CoV-2 Infection in Danish Mask Wearers. Annals of Internal Medicine. https://doi.org/10.7326/M20-6817
• A randomized controlled trial in Denmark did not demonstrate effectiveness of adding a mask recommendation to other public health measures in reducing SARS-CoV-2 infection among participants instructed to wear masks (OR = 0.82, 95% CI 0.54-1.23), and did not investigate the broader community benefits from mask wearing
dean- Posts : 5607
Join date : 2008-01-01
 Re: I do not believe it is airborn it is touch
Re: I do not believe it is airborn it is touch
https://www.nature.com/articles/s41598-020-76442-2
Long-distance airborne dispersal of SARS-CoV-2 in COVID-19 wards
Long-distance airborne dispersal of SARS-CoV-2 in COVID-19 wards
Evidence suggests that SARS-CoV-2, as well as other coronaviruses, can be dispersed and potentially transmitted by aerosols directly or via ventilation systems. We therefore investigated ventilation openings in one COVID-19 ward and central ducts that expel indoor air from three COVID-19 wards at Uppsala University Hospital, Sweden, during April and May 2020. Swab samples were taken from individual ceiling ventilation openings and surfaces in central ducts. Samples were subsequently subjected to rRT-PCR targeting the N and E genes of SARS-CoV-2. Central ventilation HEPA filters, located several stories above the wards, were removed and portions analyzed in the same manner. In two subsequent samplings, SARS-CoV-2 N and E genes were detected in seven and four out of 19 room vents, respectively. Central ventilation HEPA exhaust filters from the ward were found positive for both genes in three samples. Corresponding filters from two other, adjacent COVID-19 wards were also found positive. Infective ability of the samples was assessed by inoculation of susceptible cell cultures but could not be determined in these experiments. Detection of SARS-CoV-2 in central ventilation systems, distant from patient areas, indicate that virus can be transported long distances and that droplet transmission alone cannot reasonably explain this, especially considering the relatively low air change rates in these wards. Airborne transmission of SARS-CoV-2 must be taken into consideration for preventive measures.
dean- Posts : 5607
Join date : 2008-01-01
 Re: I do not believe it is airborn it is touch
Re: I do not believe it is airborn it is touch
here was the science behind masks pre-covid
https://www.bmj.com/content/369/bmj.m1422?utm_content=americas&utm_campaign=usage&utm_medium=cpc&utm_source=trendmd
Covid-19: What is the evidence for cloth masks?
https://www.bmj.com/content/369/bmj.m1422?utm_content=americas&utm_campaign=usage&utm_medium=cpc&utm_source=trendmd
Covid-19: What is the evidence for cloth masks?
A preprint of a rapid systematic review has assessed the current evidence on respiratory illnesses and the use of face masks (mainly surgical paper masks) in community settings.4 The paper, yet to be peer reviewed, included 31 studies, of which 12 were randomised controlled trials. The researchers reported that “wearing facemasks can be very slightly protective against primary infection from casual community contact, and modestly protective against household infections when both infected and uninfected members wear facemasks.” However, they said that many of the studies “suffered from poor compliance and controls.”
They concluded, “The evidence is not sufficiently strong to support widespread use of facemasks as a protective measure against covid-19. However, there is enough evidence to support the use of facemasks for short periods of time by particularly vulnerable individuals when in transient higher risk situations.”
dean- Posts : 5607
Join date : 2008-01-01
 skin
skin
https://journals.plos.org/plosntds/article?id=10.1371/journal.pntd.0008831
Modeling the stability of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) on skin, currency, and clothing
Modeling the stability of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) on skin, currency, and clothing
Abstract
A new coronavirus (SARS-CoV-2) emerged in the winter of 2019 in Wuhan, China, and rapidly spread around the world. The extent and efficiency of SARS-CoV-2 pandemic is far greater than previous coronaviruses that emerged in the 21st Century. Here, we modeled stability of SARS-CoV-2 on skin, paper currency, and clothing to determine if these surfaces may factor in the fomite transmission dynamics of SARS-CoV-2. Skin, currency, and clothing samples were exposed to SARS-CoV-2 under laboratory conditions and incubated at three different temperatures (4°C± 2°C, 22°C± 2°C, and 37°C ± 2°C). We evaluated stability at 0 hours (h), 4 h, 8 h, 24 h, 72 h, 96 h, 7 days, and 14 days post-exposure. SARS-CoV-2 was stable on skin through the duration of the experiment at 4°C (14 days). Virus remained stable on skin for at least 96 h at 22°C and for at least 8h at 37°C. There were minimal differences between the tested currency samples. The virus remained stable on the $1 U.S.A. Bank Note for at least 96 h at 4°C while we did not detect viable virus on the $20 U.S.A. Bank Note samples beyond 72 h. The virus remained stable on both Bank Notes for at least 8 h at 22°C and 4 h at 37°C. Clothing samples were similar in stability to the currency. Viable virus remained for at least 96 h at 4°C and at least 4 h at 22°C. We did not detect viable virus on clothing samples at 37°C after initial exposure. This study confirms the inverse relationship between virus stability and temperature. Furthermore, virus stability on skin demonstrates the need for continued hand hygiene practices to minimize fomite transmission both in the general population as well as in workplaces where close contact is common.
Author summary
A new coronavirus (SARS-CoV-2) emerged in the winter of 2019 in Wuhan, China, and rapidly spread around the world. It is still unclear why and how this particular coronavirus has spread with greater efficiency around the world than previous emerging coronaviruses. It is also unclear what potential role surfaces and direct contact have with virus transmission. We attempted to determine if SARS-CoV-2 remained infectious on a series of tested surfaces for longer periods compared with other coronaviruses. Our studies indicate that when we inoculate SARS-CoV-2 on skin, the virus can remain infectious for up for 96 hours at room temperature. Clothing and bank notes where not as hospitable for virus stability as skin across all three tested temperatures. Refrigerated conditions also enhance stability of SARS-CoV-2 across all tested surfaces. These studies demonstrate the continued need for strict public health measures to combat the ongoing pandemic particularly during cold weather months.
dean- Posts : 5607
Join date : 2008-01-01
 Re: I do not believe it is airborn it is touch
Re: I do not believe it is airborn it is touch
https://www.thelancet.com/journals/laninf/article/PIIS1473-3099(20)30833-1/fulltext
SARS-CoV-2 seroprevalence and transmission risk factors among high-risk close contacts: a retrospective cohort study
SARS-CoV-2 seroprevalence and transmission risk factors among high-risk close contacts: a retrospective cohort study
Summary
Background
The proportion of asymptomatic carriers and transmission risk factors of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) among household and non-household contacts remains unclear. In Singapore, extensive contact tracing by the Ministry of Health for every diagnosed COVID-19 case, and legally enforced quarantine and intensive health surveillance of close contacts provided a rare opportunity to determine asymptomatic attack rates and SARS-CoV-2 transmission risk factors among community close contacts of patients with COVID-19.
dean- Posts : 5607
Join date : 2008-01-01
 Re: I do not believe it is airborn it is touch
Re: I do not believe it is airborn it is touch
bars are a touch central...
https://www.nytimes.com/live/2020/10/31/world/covid-19-coronavirus?campaign_id=60&emc=edit_na_20201031&instance_id=0&nl=breaking-news&ref=headline®i_id=115919677&segment_id=43041&user_id=f730a3b9531f5b2c781c5ff7996dd05c
View in browser | nytimes.com
BREAKING NEWS
Prime Minister Boris Johnson announced plans to temporarily close pubs and restaurants in England, a day after the U.S. hit a record 99,000 new cases.
https://www.nytimes.com/live/2020/10/31/world/covid-19-coronavirus?campaign_id=60&emc=edit_na_20201031&instance_id=0&nl=breaking-news&ref=headline®i_id=115919677&segment_id=43041&user_id=f730a3b9531f5b2c781c5ff7996dd05c
View in browser | nytimes.com
BREAKING NEWS
Prime Minister Boris Johnson announced plans to temporarily close pubs and restaurants in England, a day after the U.S. hit a record 99,000 new cases.
Saturday, October 31, 2020 5:31 PM EST
The expansive new restrictions added to Europe’s growing lockdowns, with France, Germany, Belgium and Ireland shutting down large parts of their societies.
In the U.S., two dozen states reported their worst weeks for new cases.
Read the latest
dean- Posts : 5607
Join date : 2008-01-01
 Re: I do not believe it is airborn it is touch
Re: I do not believe it is airborn it is touch
jiber wrote:
Consider, Wyllie says, the extraordinary chain of events that would need to happen to successfully spread SARS-CoV-2 on a surface. A sufficiently large amount of the virus would need to be sprayed by an infected person onto a surface. The surface would need to be the right kind of material, exposed to the right levels of light, temperature, and humidity so that the virus does not quickly degrade. Then the virus would need to be picked up—which you would most likely do with your hands. But the virus is vulnerable there. (“Enveloped” viruses like SARS-CoV-2 do not fare well on porous surfaces like skin and clothing.) And then it needs to find a way inside you—usually through your nose or your eye—in a concentration big enough to get past your mucosal defenses and establish itself in your cells. The risk, Wyllie concludes, is low. “I’ve not once washed my groceries or disinfected my bags or even thought twice about my mail,” she says.
shame on her Wyllie for anecdotal ... that is irresponsible science/ behavior. but she claims it is only sprayed... she does not contemplate touching ones own mucous orifices after coughing sneezing. Other past viruses have been shown to be on surfaces.
please read the documentation. Do you realize a computer keyboard harbors 400 times more germs than a toilet seat. A human touches their face 23 times an hour is how a keyboard , light switch door knob and so on have higher viral loads than air in hospitals.
On a metal door knob or plastic keyboard or plastic light switch elevator button or metal bus handle to get into the transport, the back of a metal chair, the life of covid is up to was it 3 days?
It is as simple as this, yout touch your face 23 times an hour. Half of those are touching a mucous part that if infected allows your hand to deposit the virus on any item you later touch. Then again if not ill you touch a light switch or anything else a infected person touches, then you in your 23 times an hour touch your face and half of them a mucous surface which is the way the virus can infect you.
Note as you touch your face 23 times an hour and you hug or kiss in a greeting an infected person. It is on your face and now in 50% of your hourly face touching you get it on your hands. Then in the other half of the 23 times an hour you then touch mucous that now can cause infection.
All te above at rates of 23 times an hour meet the 3 days covid can last on plastic or metal.
Can COVID-19 live on surfaces?
In a study by the U.S. National Institutes of Health (NIH), researchers found that the virus that causes COVID-19 can live up to four hours on copper, up to 24 hours on cardboard, and up to three days on stainless steel and plastic surfaces.
and here is the link for Wyllie who does note it is not settled science still, again cough and touch your face 23 times an hour. touch a surface like keyboard, remote control, door handle, light switch, fridge handle, coffee pot, a hug kiss. pass it on...
https://www.wired.com/story/its-time-to-talk-about-covid-19-and-surfaces-again/
https://www.sciencedirect.com/science/article/pii/S1438463918305911
Impact of a hygiene intervention on virus spread in an office building
Abstract
Viral illnesses have a significant direct and indirect impact on the workplace that burdens employers with increased healthcare costs, low productivity, and absenteeism. Workers' direct contact with each other and contaminated surfaces contributes to the spread of viruses at work. This study quantifies the impact of an office wellness intervention (OWI) to reduce viral load in the workplace. The OWI includes the use of a spray disinfectant on high-touch surfaces and providing workers with alcohol-based hand sanitizer gel and hand sanitizing wipes along with user instructions. Viral transmission was monitored by applying an MS2 phage tracer to a door handle and the hand of a single volunteer participant. At the same time, a placebo inoculum was applied to the hands of four additional volunteers. The purpose was to evaluate the concentration of viruses on workers' hands and office surfaces before and after the OWI. Results showed that the OWI significantly reduced viable phage concentrations per surface area on participants' hands, shared fomites, and personal fomites (p = 0.0001) with an 85.4% average reduction. Reduction of virus concentrations on hands and fomites is expected to subsequently minimize the risk of infections from common enteric and respiratory pathogens. The surfaces identified as most contaminated were the refrigerator, drawer handles and sink faucets in the break room, along with pushbar on the main exit of the building, and the soap dispensers in the women's restroom. A comparison of contamination in different locations within the office showed that the break room and women's restrooms were the sites with the highest tracer counts. Results of this study can be used to inform quantitative microbial risk assessment (QMRA) models aimed at defining the relationship between surface contamination, pathogen exposure and the probability of disease that contributes to high healthcare costs, absenteeism, presenteeism, and loss of productivity in the workplace.
https://www.sciencedirect.com/science/article/pii/S1438463918305911
Impact of a hygiene intervention on virus spread in an office building
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4455933/
Modeling of Human Viruses on Hands and Risk of Infection in an Office Workplace Using Micro-Activity Data
https://academic.oup.com/cid/advance-article/doi/10.1093/cid/ciaa1517/5917611
https://www.tandfonline.com/doi/full/10.1080/15459624.2019.1691219?src=recsys
Assessing virus infection probability in an office setting using stochastic simulation
https://pubmed.ncbi.nlm.nih.gov/26066784/
The healthy workplace project: Reduced viral exposure in an office setting
https://pubmed.ncbi.nlm.nih.gov/32574546/
Evaluating a transfer gradient assumption in a fomite-mediated microbial transmission model using an experimental and Bayesian approach
https://pubmed.ncbi.nlm.nih.gov/32329918/
Bacterial transfer to fingertips during sequential surface contacts with and without gloves
https://pubmed.ncbi.nlm.nih.gov/12234341/
Comparative surface-to-hand and fingertip-to-mouth transfer efficiency of gram-positive bacteria, gram-negative bacteria, and phage
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4455933/
Modeling of Human Viruses on Hands and Risk of Infection in an Office Workplace Using Micro-Activity Data
dean- Posts : 5607
Join date : 2008-01-01
 Re: I do not believe it is airborn it is touch
Re: I do not believe it is airborn it is touch
note the 2 refs did not catch it, they were breathing the same air.
https://www.cdc.gov/mmwr/volumes/69/wr/mm6941a4.htm?s_cid=mm6941a4_w
An Outbreak of COVID-19 Associated with a Recreational Hockey Game — Florida, June 2020
https://www.cdc.gov/mmwr/volumes/69/wr/mm6941a4.htm?s_cid=mm6941a4_w
An Outbreak of COVID-19 Associated with a Recreational Hockey Game — Florida, June 2020
On June 16, 2020, a recreational ice hockey game was played at an ice rink in the Tampa Bay, Florida, metropolitan area. Teams A and B, each consisting of 11 players (typically six on the ice and five on the bench at any given time), included men aged 19–53 years. During the 5 days after the game, 15 persons (14 of the 22 players and a rink staff member) experienced signs and symptoms compatible with coronavirus disease 2019 (COVID-19)*; 13 of the 15 ill persons had positive laboratory test results indicating infection with SARS-CoV-2, the virus that causes COVID-19. Widespread transmission of SARS-CoV-2 has been documented at a choir practice (1) and at meat processing plants (2,3); however, apart from an outbreak involving 57 infected dancers that has been linked to high-intensity fitness dance classes in South Korea (4) and a cluster of five infected persons at a squash facility in Slovenia (5), few published reports are available regarding transmission associated with specific sports games or practices. In addition, outbreaks of COVID-19 infections among amateur hockey players in the United States have recently been reported in the news.†
On June 19, 2020, the Florida Department of Health was notified of a team A player (the index patient) who experienced fever, cough, sore throat, and a headache beginning on June 17, the day after he had participated in an evening game; 2 days later, a nasal specimen was obtained, which tested positive for SARS-CoV-2 by Sofia SARS Antigen Fluorescent Immunoassay (https://www.quidel.com/immunoassays/coronavirusexternal icon). An investigation by the Florida Department of Health revealed that eight of 10 team A players (excluding the index patient), five of 11 players from team B, and one rink staff member experienced COVID-19 signs and symptoms during June 18–21 (Figure), 2–5 days after the game. Excluding the index patient, 13 of the 21 (62%) players experienced illness. Among the 15 total cases in this outbreak, 11 patients had positive SARS-CoV-2 reverse transcription–polymerase chain reaction results, two had positive antigen tests,§ and two were not tested.¶ Asymptomatic players did not seek testing. Neither of the two on-ice referees experienced symptoms. Because the investigation was deemed public health practice, approval by the Florida Department of Health Institutional Review Board was not required.
dean- Posts : 5607
Join date : 2008-01-01
 You are wrong - Covid is airborne
You are wrong - Covid is airborne
Consider, Wyllie says, the extraordinary chain of events that would need to happen to successfully spread SARS-CoV-2 on a surface. A sufficiently large amount of the virus would need to be sprayed by an infected person onto a surface. The surface would need to be the right kind of material, exposed to the right levels of light, temperature, and humidity so that the virus does not quickly degrade. Then the virus would need to be picked up—which you would most likely do with your hands. But the virus is vulnerable there. (“Enveloped” viruses like SARS-CoV-2 do not fare well on porous surfaces like skin and clothing.) And then it needs to find a way inside you—usually through your nose or your eye—in a concentration big enough to get past your mucosal defenses and establish itself in your cells. The risk, Wyllie concludes, is low. “I’ve not once washed my groceries or disinfected my bags or even thought twice about my mail,” she says.
jiber- Posts : 1
Join date : 2020-10-25
 airflow simulation it goes forward.
airflow simulation it goes forward.
though to me this seems obvious if sitting on a seat on a plane your airflow you project is forward towards the person sitting in front of you. Thus the people sitting in front of you if you are infected if airborne would definitely have a higher infection rated tahn the people sitting next to you. plus the way a plane ventilation words it would also propel it directly at you as it rises that way.
But wesee that in the study of infected people in average 2 hour were the persons next to them at a low rate of 3.6% and the person in front of them the direction the particles are going is half of that.
Supercomputer Shows Humidity's Effect on COVID-19
https://youtu.be/frbsdgGMHew
But wesee that in the study of infected people in average 2 hour were the persons next to them at a low rate of 3.6% and the person in front of them the direction the particles are going is half of that.
Supercomputer Shows Humidity's Effect on COVID-19
https://youtu.be/frbsdgGMHew
Last edited by dean on Sun Feb 21, 2021 9:09 pm; edited 1 time in total
dean- Posts : 5607
Join date : 2008-01-01
 Re: I do not believe it is airborn it is touch
Re: I do not believe it is airborn it is touch
peer reviewed the guard always had a mask on. but you see that they have to make contact with the food trays and the bedding.
https://www.cdc.gov/mmwr/volumes/69/wr/mm6943e1.htm?s_cid=mm6943e1_w
COVID-19 in a Correctional Facility Employee Following Multiple Brief Exposures to Persons with COVID-19 — Vermont, July–August 2020
https://www.cdc.gov/mmwr/volumes/69/wr/mm6943e1.htm?s_cid=mm6943e1_w
COVID-19 in a Correctional Facility Employee Following Multiple Brief Exposures to Persons with COVID-19 — Vermont, July–August 2020
On August 11, 2020, a confirmed case of coronavirus disease 2019 (COVID-19) in a male correctional facility employee (correctional officer) aged 20 years was reported to the Vermont Department of Health (VDH). On July 28, the correctional officer had multiple brief encounters with six incarcerated or detained persons (IDPs)* while their SARS-CoV-2 test results were pending. The six asymptomatic IDPs arrived from an out-of-state correctional facility on July 28 and were housed in a quarantine unit. In accordance with Vermont Department of Corrections (VDOC) policy for state prisons, nasopharyngeal swabs were collected from the six IDPs on their arrival date and tested for SARS-CoV-2, the virus that causes COVID-19, at the Vermont Department of Health Laboratory, using real-time reverse transcription–polymerase chain reaction (RT-PCR). On July 29, all six IDPs received positive test results. VDH and VDOC conducted a contact tracing investigation† and used video surveillance footage to determine that the correctional officer did not meet VDH’s definition of close contact (i.e., being within 6 feet of infectious persons for ≥15 consecutive minutes)§,¶; therefore, he continued to work. At the end of his shift on August 4, he experienced loss of smell and taste, myalgia, runny nose, cough, shortness of breath, headache, loss of appetite, and gastrointestinal symptoms; beginning August 5, he stayed home from work. An August 5 nasopharyngeal specimen tested for SARS-CoV-2 by real-time RT-PCR at a commercial laboratory was reported as positive on August 11; the correctional officer identified two contacts outside of work, neither of whom developed COVID-19. On July 28, seven days preceding his illness onset, the correctional officer had multiple brief exposures to six IDPs who later tested positive for SARS-CoV-2; available data suggests that at least one of the asymptomatic IDPs transmitted SARS-CoV-2 during these brief encounters.
Subsequently, VDH and facility staff members reviewed July 28 quarantine unit video surveillance footage and standard correctional officer shift duty responsibilities to approximate the frequency and duration of interactions between the correctional officer and infectious IDPs during the work shift (Table). Although the correctional officer never spent 15 consecutive minutes within 6 feet of an IDP with COVID-19, numerous brief (approximately 1-minute) encounters that cumulatively exceeded 15 minutes did occur. During his 8-hour shift on July 28, the correctional officer was within 6 feet of an infectious IDP an estimated 22 times while the cell door was open, for an estimated 17 total minutes of cumulative exposure. IDPs wore microfiber cloth masks during most interactions with the correctional officer that occurred outside a cell; however, during several encounters in a cell doorway or in the recreation room, IDPs did not wear masks. During all interactions, the correctional officer wore a microfiber cloth mask, gown, and eye protection (goggles). The correctional officer wore gloves during most interactions. The correctional officer’s cumulative exposure time is an informed estimate; additional interactions might have occurred that were missed during this investigation.
The correctional officer reported no other known close contact exposures to persons with COVID-19 outside work and no travel outside Vermont during the 14 days preceding illness onset. COVID-19 cumulative incidence in his county of residence and where the correctional facility is located was relatively low at the time of the investigation (20 cases per 100,000 persons), suggesting that his most likely exposures occurred in the correctional facility through multiple brief encounters (not initially considered to meet VDH’s definition of close contact exposure) with IDPs who later received a positive SARS-CoV-2 test result.
Among seven employees with exposures to the infectious IDPs that did meet the VDH close contact definition, one person received a positive test result. Among thirteen employees (including the correctional officer) with exposures to the infectious IDPs that did not meet the VDH close contact definition during contact tracing, only the correctional officer received a positive SARS-CoV-2 test result.
Data are limited to precisely define “close contact”; however, 15 minutes of close exposure is used as an operational definition for contact tracing investigations in many settings. Additional factors to consider when defining close contact include proximity, the duration of exposure, whether the infected person has symptoms, whether the infected person was likely to generate respiratory aerosols, and environmental factors such as adequacy of ventilation and crowding. A primary purpose of contact tracing is to identify persons with higher risk exposures and therefore higher probabilities of developing infection, which can guide decisions on quarantining and work restrictions. Although the initial assessment did not suggest that the officer had close contact exposures, detailed review of video footage identified that the cumulative duration of exposures exceeded 15 minutes. In correctional settings, frequent encounters of ≤6 feet between IDPs and facility staff members are necessary; public health officials should consider transmission-risk implications of cumulative exposure time within such settings.
dean- Posts : 5607
Join date : 2008-01-01
 Re: I do not believe it is airborn it is touch
Re: I do not believe it is airborn it is touch
if airborne there is no way this number would be this low. after all when you enter a plane you are breathing and exhaling.
https://finance.yahoo.com/news/risk-inflight-spread-covid-19-133425365.html
Risk of inflight spread of COVID-19 'very low', not zero: WHO
https://finance.yahoo.com/news/risk-inflight-spread-covid-19-133425365.html
Risk of inflight spread of COVID-19 'very low', not zero: WHO
GENEVA (Reuters) - The risk of COVID-19 spreading on flights appears "very low" but cannot be ruled out, despite studies showing only a small number of cases, the World Health Organization (WHO) said.
"In-flight transmission is possible but the risk appears to be very low, given the volume of travellers and the small number of case reports. The fact that transmission is not widely documented in the published literature does not, however, mean it does not happen," the WHO said in a statement to Reuters.
The characterisation of the risk echoes the findings of a U.S. Defense Department study that last week described the probability of catching the disease on airliners as "very low".
Some airlines have however used more robust language to describe the risk of onboard transmission.
Southwest Airlines and United Airlines have both said that recent studies had found that the risk was "virtually non-existent".
Southwest, one of a handful of airlines currently keeping middle seats free, said on Thursday that in light of the research it would lift the block on middle seats.
Global airlines body IATA said on Oct. 8 that only 44 potential cases of flight-related transmission had been identified among 1.2 billion travellers this year, or one in every 27 million passengers.
But the presentation was later challenged by one of the scientists whose research it drew upon.
dean- Posts : 5607
Join date : 2008-01-01
 Sweden
Sweden
https://news.yahoo.com/as-white-house-eyes-herd-immunity-swedens-nomask-approach-is-failing-to-contain-covid-19-151813672.html
With infection rates now rising in Sweden — though not to the extremes of countries such as Spain, France, Belgium and the U.K. —and for youth to stop partying, all factors blamed for the uptick in cases to more than 600 a day, up from around 100 at summer’s end.the Swedish prime minister himself recently implored his countrymen to stop hugging and kissing their friends,
Last edited by dean on Sat Nov 21, 2020 8:12 am; edited 1 time in total
dean- Posts : 5607
Join date : 2008-01-01
 Re: I do not believe it is airborn it is touch
Re: I do not believe it is airborn it is touch
https://www.tandfonline.com/doi/full/10.1080/15459624.2013.877591?src=recsys
Efficacy of Face Shields Against Cough Aerosol Droplets from a Cough Simulator
[quote]
[/b]
https://www.tandfonline.com/doi/full/10.1080/02786826.2020.1749229?src=recsys
Editorial
The coronavirus pandemic and aerosols: Does COVID-19 transmit via expiratory particles?
Sima Asadi,Nicole Bouvier,Anthony S. Wexler &William D. Ristenpart
Pages 635-638 | Received 26 Mar 2020, Accepted 26 Mar 2020, Published online: 03 Apr 2020
Efficacy of Face Shields Against Cough Aerosol Droplets from a Cough Simulator
[quote]
[/b]
Health care workers are exposed to potentially infectious airborne particles while providing routine care to coughing patients. However, much is not understood about the behavior of these aerosols and the risks they pose. We used a coughing patient simulator and a breathing worker simulator to investigate the exposure of health care workers to cough aerosol droplets, and to examine the efficacy of face shields in reducing this exposure. Our results showed that 0.9% of the initial burst of aerosol from a cough can be inhaled by a worker 46 cm (18 inches) from the patient. During testing of an influenza-laden cough aerosol with a volume median diameter (VMD) of 8.5 μm, wearing a face shield reduced the inhalational exposure of the worker by 96% in the period immediately after a cough. The face shield also reduced the surface contamination of a respirator by 97%. When a smaller cough aerosol was used (VMD = 3.4 μm), the face shield was less effective, blocking only 68% of the cough and 76% of the surface contamination. In the period from 1 to 30 minutes after a cough, during which the aerosol had dispersed throughout the room and larger particles had settled, the face shield reduced aerosol inhalation by only 23%. Increasing the distance between the patient and worker to 183 cm (72 inches) reduced the exposure to influenza that occurred immediately after a cough by 92%. Our results show that health care workers can inhale infectious airborne particles while treating a coughing patient. Face shields can substantially reduce the short-term exposure of health care workers to large infectious aerosol particles, but smaller particles can remain airborne longer and flow around the face shield more easily to be inhaled. Thus, face shields provide a useful adjunct to respiratory protection for workers caring for patients with respiratory infections. However, they cannot be used as a substitute for respiratory protection when it is needed.
https://www.tandfonline.com/doi/full/10.1080/02786826.2020.1749229?src=recsys
Editorial
The coronavirus pandemic and aerosols: Does COVID-19 transmit via expiratory particles?
Sima Asadi,Nicole Bouvier,Anthony S. Wexler &William D. Ristenpart
Pages 635-638 | Received 26 Mar 2020, Accepted 26 Mar 2020, Published online: 03 Apr 2020
dean- Posts : 5607
Join date : 2008-01-01
 Re: I do not believe it is airborn it is touch
Re: I do not believe it is airborn it is touch
We know from previous published real world that on a plane with 6 infected not all wore masks 1-2 person got infected in 11 hour flight. and from bullet train before masks about 70,000 contact tracing 400-600 infected chances of infection sitting next to infected in average 2 hour ride 3.6%, in front of them the way you are breathing half of that. now we have a simulation wearing masks shows nearly impossible by air. But they did not test contact, but united sprays their planes with a contact coating that minimizes this for up to 30-90 days. So if you wash your hands your risk is so low.
below is up for peer review, not peer reviewed yet.
https://abcnews.go.com/Politics/risk-covid-19-exposure-planes-virtually-nonexistent-masked/story?id=73616599
Risk of COVID-19 exposure on planes 'virtually nonexistent' when masked, study shows
It was conducted by the Department of Defense and United Airlines.
ByGio Benitez andSam Sweeney
https://nationalpost.com/news/world/coughing-mannequins-put-to-work-as-boeing-united-airlines-try-to-figure-out-how-covid-moves-through-planes
Coughing mannequins put to work as Boeing, United Airlines try to figure out how COVID moves through planes
below is up for peer review, not peer reviewed yet.
https://abcnews.go.com/Politics/risk-covid-19-exposure-planes-virtually-nonexistent-masked/story?id=73616599
Risk of COVID-19 exposure on planes 'virtually nonexistent' when masked, study shows
It was conducted by the Department of Defense and United Airlines.
ByGio Benitez andSam Sweeney
United Airlines says the risk of COVID-19 exposure onboard its aircraft is "virtually non-existent" after a new study finds that when masks are worn there is only a 0.003% chance particles from a passenger can enter the passenger's breathing space who is sitting beside them.
The study, conducted by the Department of Defense in partnership with United Airlines, was published Thursday. They ran 300 tests in a little over six months with a mannequin on a United plane.
PHOTO: The U.S. Department of Defense published a study Wednesday on cabin airflow that found when a passenger is seated and wearing a mask, only 0.001% of infected air particles could enter their breathing zone.
The U.S. Department of Defense published a study Wednesday on cabin airflow that found when a passenger is seated and wearing a mask, only 0.001% of infected air particles could enter their breathing zone.
The mannequin was equipped with an aerosol generator that allowed technicians to reproduce breathing and coughing. Each test released 180 million particles - equivalent to the number of particles that would be produced by thousands of coughs. They studied the way the mannequin's particles moved inside the cabin with a mask on and off.
The tests assumed the flight was completely full with technicians placing sensors in seats, galleys, and the jet bridge to represent other passengers on the plane.
MORE: US airline launches first COVID-19 testing program of its kind
"99.99% of those particles left the interior of the aircraft within six minutes," United Airlines Chief Communication Officer Josh Earnest told ABC News. "It indicates that being on board an aircraft is the safest indoor public space, because of the unique configuration inside an aircraft that includes aggressive ventilation, lots of airflow."
In late September, major U.S. airline CEOs said their employees were reporting lower rates of COVID-19 infection than the general public.
MORE: US airline employees report lower rate of COVID-19 infection than public, CEOs say
"At United, but also at our large competitors, our flight attendants have lower COVID infection rates than the general population, which is one of multiple data points that speaks to the safety on board airplanes," United Airlines CEO Scott Kirby said during a Politico event.
Last week, the International Air Transport Association (IATA) released new research, saying the risk of contracting the virus on a plane appears to be "in the same category as being struck by lightning."
PHOTO: The U.S. Department of Defense published a study Wednesday on cabin airflow that found when a passenger is seated and wearing a mask, only 0.001% of infected air particles could enter their breathing zone.
The U.S. Department of Defense published a study Wednesday on cabin airflow that found when a passenger is seated and wearing a mask, only 0.001% of infected air particles could enter their breathing zone.
Among 1.2 billion travelers, IATA found only 44 published cases of potential inflight transmission. Most of those 44 cases occurred in the early days of the pandemic when masks were not required.
Air travel is still down around 70 percent compared to last year, but there has been an uptick since the spring. Earlier this week the Transportation Security Administration (TSA) screened nearly a million people at U.S. airports - the agency's highest number since mid-March.
"We're seeing recovery, but we have a long way to go," Earnest said. "And even with all of this promising information about the safety of air travel and some of the advances that we're making in terms of implementing a testing regimen - we recognize we're not going to be anywhere close to back to normal until we have a vaccine that's been widely distributed and administered."
https://nationalpost.com/news/world/coughing-mannequins-put-to-work-as-boeing-united-airlines-try-to-figure-out-how-covid-moves-through-planes
Coughing mannequins put to work as Boeing, United Airlines try to figure out how COVID moves through planes
For the past four months, United Airlines Holdings Inc. and Boeing Co. have been flying around jetliners loaded with mannequins, aerosol sprays, sensors and scientists in an effort to understand how contaminated air moves through passenger planes.
The research is just one small part of a sweeping global campaign to figure out the threats posed by the coronavirus. But for the airline industry, the results could help determine how quickly carriers bounce back from the edge of disaster after the pandemic made people afraid to get on a plane. U.S. demand for flights remains at less than a third of 2019 levels, based on airport security screening data.
The U.S. military initiated the $1 million study when the spread of COVID-19 raised concerns about infection risks for troops transported on passenger jets. Companies including United, Boeing and Zeteo Tech LLC, a Maryland-based biodefense and medical device maker, are contributing equipment and expertise. If the findings can show how likely it is for a passenger to be infected by breathing the air on a plane, “it’ll probably drive some policy decisions,” said Mike McLoughlin, Zeteo’s vice president of research.
Advertisement
Article content continued
Airlines have sought to reassure the public that flying is safe by implementing an array of onboard cleaning and disinfecting procedures, requiring face masks in the cabin and improving ventilation and filtration systems. But they haven’t been able to show what, precisely, are the chances of infection if that person sitting next to you or across the aisle breaks out into a virus-laden cough.
To collect the data, researchers placed mannequins with human-like heads in various seats throughout seven models of Boeing and Airbus SE jets, then made them cough. Or rather, they simulated a human cough, and how aerosolized particles are expelled and disseminated through the air on the plane, McLoughlin said.
Aerosol particles will behave differently under different cabin scenarios, said Byron Jones, an engineering professor at Kansas State University who studies airline cabin air and was not involved in the project. Gas and particles in a cabin become “a witches’ cauldron,” he said, based on air flows, particulate sizes and other factors. “It just swirls and churns and twists. It’s very chaotic,” he said. But that churning isn’t necessarily a bad thing: “That’s what you want to see in a general ventilation (system).”
The Seattle innovation company has developed a technology that will literally shield travellers from the virus as they board airplanes for the first time.
Flying during COVID-19: How a 3D-printed device could shield travellers on board airplanes
While they are calling on the government to ease restrictions, he said they still expect it will be a long way before things return to normal.
'We can’t wait years': Airlines tell MPs they want COVID-19 rules eased so their business can restart
A traveller wears a face covering as he walks through a mostly empty terminal at Ronald Reagan Washington National Airport, May 5, 2020 in Arlington, Virginia.
Flying in the post-lockdown world: What might that look like?
Advertisement
Article content continued
Researchers evaluated how factors such as circulation, the exchange rate of cabin air, filtration and forward-facing seats affected the flow of aerosolized particles through the cabin, and who would be most exposed in their proximity to a cougher. Particle sizes and various locations throughout the cabin were considered. Tests were repeated with the dummies wearing disposable surgical masks.
The tests were conducted during 30 hours in flight and 24 hours on the ground from May 5 through August. Analysis of the data and peer reviews are expected to be completed this month with a final report issued in October.
Boeing declined to comment on the results they’ve seen so far. In a statement, the company said it’s approaching the question of virus spread “from an engineering perspective by conducting data-driven analysis studies, simulations, modeling and live testing, which will help us all better understand the transmission and risks of COVID-19.”
The project is funded and led in part by the U.S. Transportation Command, based at Scott Air Force Base in Illinois, which buys airline seats and charter flights to transport U.S. troops and their families around the world. The Command sees the study as critical to safely mobilizing troops, said Lieutenant Colonel Ellis Gales Jr., a spokesman. The Defense Advanced Research Projects Agency helped connect the Transportation Command with United and Boeing.
If the analysis shows infection risks through the air can be controlled on a plane, the industry might be able to use those results to help persuade the public to start flying again even before a vaccination for COVID-19 might be widely available.”Throughout the pandemic, our top priority has been the health and safety of our customers and crew,” Toby Enqvist, United’s chief customer officer, said in an email. Enqvist said he’s encouraged by the early results he’s seen, but did not provide specifics.
“Everybody is keen to get the results out as quickly as possible but we want to make sure that when we release those results we’re painting an accurate picture,” McLoughlin said.
dean- Posts : 5607
Join date : 2008-01-01
 Re: I do not believe it is airborn it is touch
Re: I do not believe it is airborn it is touch
https://academic.oup.com/annweh/article/52/5/351/167261
Visualization of the Airflow around a Life-Sized, Heated, Breathing Mannequin at Ultralow Windspeeds
Visualization of the Airflow around a Life-Sized, Heated, Breathing Mannequin at Ultralow Windspeeds
dean- Posts : 5607
Join date : 2008-01-01
 Re: I do not believe it is airborn it is touch
Re: I do not believe it is airborn it is touch
here is a very good one for showing c-19 was not in the air but on surfaces several days after diagnosis. Note this is peer reviewed science. testing feb 6- april 10 and just published.
https://journals.plos.org/plosntds/article?id=10.1371/journal.pntd.0008570
Air and surface contamination in non-health care settings among 641 environmental specimens of 39 COVID-19 cases
Abstract
Little is known about the SARS-CoV-2 contamination of environmental surfaces and air in non-health care settings among COVID-19 cases. We explored the SARS-CoV-2 contamination of environmental surfaces and air by collecting air and swabbing environmental surfaces among 39 COVID-19 cases in Guangzhou, China. The specimens were tested on RT-PCR. The information collected for COVID-19 cases included basic demographic, clinical severity, symptoms at onset, radiological testing, laboratory testing and hospital admission. A total of 641 environmental surfaces and air specimens were collected among 39 COVID-19 cases before disinfection. Among them, 20 specimens (20/641, 3.1%) were tested positive from 9 COVID-19 cases (9/39, 23.1%), with 5 (5/101, 5.0%) positive specimens from 3 asymptomatic cases, 5 (5/220, 2.3%) from 3 mild cases, and 10 (10/374, 2.7%) from 3 moderate cases. All positive specimens were collected within 3 days after diagnosis, and 10 (10/42, 23.8%) were found in toilet (5 on toilet bowl, 4 on sink/faucet/shower, 1 on floor drain), 4 (4/21, 19.0%) in anteroom (2 on water dispenser/cup/bottle, 1 on chair/table, 1 on TV remote), 1 (1/8, 12.5%) in kitchen (1 on dining-table), 1 (1/18, 5.6%) in bedroom (1 on bed/sheet pillow/bedside table), 1 (1/5, 20.0%) in car (1 on steering wheel/seat/handlebar) and 3 (3/20, 21.4%) on door knobs. Air specimens in room (0/10, 0.0%) and car (0/1, 0.0%) were all negative. SARS-CoV-2 was found on environmental surfaces especially in toilet, and may survive for several days. We provided evidence of potential for SARS-CoV-2 transmission through contamination of environmental surfaces.
Author summary
The Coronavirus Disease 2019 (COVID-19) pandemic has precipitated a global crisis. It is important to understanding the SARS-CoV-2 contamination of environmental surfaces and air in non-health care settings among COVID-19 cases. In this study, we explored the SARS-CoV-2 contamination of environmental surfaces and air by collecting air and swabbing environmental surfaces among 39 COVID-19 cases in Guangzhou, China. We found that 20 specimens were tested positive from 9 COVID-19 cases. All positive specimens were collected within 3 days after diagnosis, and 10 were found in toilet. Air specimens in room and car were all negative. SARS-CoV-2 was found on environmental surfaces especially in toilet, and may survive for several days. We provided evidence of potential for SARS-CoV-2 transmission through contamination of environmental surfaces.
Introduction
The Coronavirus Disease 2019 (COVID-19) pandemic has precipitated a global crisis, and it has resulted in 5,404,512 confirmed cases including with 343,514 deaths globally as of May 26, 2020 [1]. Reported transmission modes of Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) among humans were mainly through respiratory droplets produced by infected cases with sneezes or coughs [2]. People may be infected by inhalation of virus laden liquid droplets, and infection is more likely when someone are in close contact with COVID-19 cases [2–4]. However, the importance of indirect contact transmission, such as environmental contamination, is uncertain [5–7]. Evidences suggested that environmental contamination with SARS-CoV-2 is likely to be high, and it is supported by recent researches focused on environmental contamination from COVID-19 cases in hospital [5–9]. Hospitals have already perfect disinfection measures, and are less likely to appear super-spreaders compared with community and household [4,10–12]. However, the role of air and surface contamination in non-health care settings is still need to be explored. Therefore, it is important to understand the environmental contamination of infected cases by SARS-CoV-2 in non-health care settings, which is a vital aspect of controlling the spread of the epidemic.
To address this question, in this study, we sampled total of 641 surfaces environmental and air specimens among 39 cases in Guangzhou, China, to explore the surrounding environmental surfaces and air contamination by SARS-CoV-2 in non-health care settings.
Methods
Study design and setting
Based on COVID-19 case reports, environmental surfaces and air specimens were collected by Guangzhou CDC (GZCDC) from Feb 6 to Apr 10, 2020. The environmental surfaces specimens of COVID-19 cases sampled in home, hotel, public area, restaurant, marketplace, car and pet, which was associated with COVID-19 cases’ life trajectory before hospitalization. Air specimens of COVID-19 cases were also sampled in their room (home or hotel). All specimens were collected before disinfection.
dean- Posts : 5607
Join date : 2008-01-01
 Re: I do not believe it is airborn it is touch
Re: I do not believe it is airborn it is touch
japan uses the worst masks and does just fine.
https://www.medrxiv.org/content/10.1101/2020.10.05.20207241v1
• [Pre-print, not peer-reviewed] Face coverings were found to be more effective than face shields at blocking the small aerosol particles propelled by a cough aerosol simulator. The efficacy of blocking aerosols was 99% with an N95 respirator, 59% with a procedure mask, 51% with a 3-ply cloth face mask, 47% with a polyester neck gaiter and 2% with a face shield.
https://www.medrxiv.org/content/10.1101/2020.10.05.20207241v1
• [Pre-print, not peer-reviewed] Face coverings were found to be more effective than face shields at blocking the small aerosol particles propelled by a cough aerosol simulator. The efficacy of blocking aerosols was 99% with an N95 respirator, 59% with a procedure mask, 51% with a 3-ply cloth face mask, 47% with a polyester neck gaiter and 2% with a face shield.
Face masks are recommended to reduce community transmission of SARS CoV 2. One of the primary benefits of face masks and other coverings is as source control devices to reduce the expulsion of respiratory aerosols during coughing, breathing, and speaking. Face shields have been proposed as an alternative to face masks, but information about face shields as source control devices is limited. We used a cough aerosol simulator with a headform to propel small aerosol particles (0 to 7 μm) into different face coverings. An N95 respirator blocked 99% of the cough aerosol, a procedure mask blocked 59%, a 3-ply cloth face mask blocked 51%, and a polyester neck gaiter blocked 47% as a single layer and 60% when folded into a double layer. In contrast, the face shield blocked 2% of the cough aerosol. Our results suggest that face masks and neck gaiters are preferable to face shields as source control devices for cough aerosols.
dean- Posts : 5607
Join date : 2008-01-01
 Re: I do not believe it is airborn it is touch
Re: I do not believe it is airborn it is touch
https://academic.oup.com/cid/advance-article/doi/10.1093/cid/ciaa1517/5917611
Survival of SARS-CoV-2 and influenza virus on the human skin: Importance of hand hygiene in COVID-19
Survival of SARS-CoV-2 and influenza virus on the human skin: Importance of hand hygiene in COVID-19
• Survival time of SARS-CoV-2 on human skin was significantly longer than that of influenza A virus (9.0 hours vs. 1.8 hours). Exposure of both viruses to 80% ethanol while on the skin surface, in the context of droplets from a cough or sneeze, inactivated both viruses within 15 seconds of exposure, indicating appropriate hand hygiene using ethanol-based disinfectants may lead to the quick viral inactivation and may reduce the high risk of contact infections.
dean- Posts : 5607
Join date : 2008-01-01
 Re: I do not believe it is airborn it is touch
Re: I do not believe it is airborn it is touch
again contsact, as I have said from the getgo, bars are huge contact areas.
https://finance.yahoo.com/news/paris-shuts-bars-brake-covid-114550310.html
Paris shuts bars to brake Covid-19 spread
https://finance.yahoo.com/news/paris-shuts-bars-brake-covid-114550310.html
Paris shuts bars to brake Covid-19 spread
dean- Posts : 5607
Join date : 2008-01-01
 Re: I do not believe it is airborn it is touch
Re: I do not believe it is airborn it is touch
https://www.route-fifty.com/health-human-services/2020/09/overlooked-variable-key-pandemic/168909/
I find it amazing that a professor writes an entire article claiming it is airborne without any discussion how he knows it is when the WHO still to this date does not claim it is with their top experts who see any documentation there is and has been for 60 plus years.
Plus he does not explain how you can sit next to with no mask on a train with 70,000 contact tracings done and 400 infected and be next to them for 2 hour average with the person next to you only 3.5% chance, and the direction you are breathing the seats in front of you half of that.
Again there is not one scientifically peer reviewed document to date that has eliminated the contact before making their claim. Till you can rule out all the potential contact you can not claim in a situation that it is airborne.
In his Japan discussion he does not even note how you do not embrace as a culture for a greeting, you get a clean hot towel in a restaurant when you are going to eat, vs the Latin American cultures that still do the kiss hug greeting. Sapin is a kiss hug culture. France is a kiss hug culture.
For the italy ones too I bet that region was known for the kiss hug greeting, and after a while they realized it and the rest of the country stopped doing it. That would easily explain the significant differentials if one was open minded about contact.
and yes UK with their bars are open as I have mentioned in a bar drinking you make mistakes the more you drink and there are so many cross contact areas there.
Sweeden and netherlands just did nothing basically.
If you look at what I just mentioned for high contact cultures from bars to kiss hug other than the USA we probably have the top 20 highest rate nations.
I find it amazing that a professor writes an entire article claiming it is airborne without any discussion how he knows it is when the WHO still to this date does not claim it is with their top experts who see any documentation there is and has been for 60 plus years.
Plus he does not explain how you can sit next to with no mask on a train with 70,000 contact tracings done and 400 infected and be next to them for 2 hour average with the person next to you only 3.5% chance, and the direction you are breathing the seats in front of you half of that.
Again there is not one scientifically peer reviewed document to date that has eliminated the contact before making their claim. Till you can rule out all the potential contact you can not claim in a situation that it is airborne.
In his Japan discussion he does not even note how you do not embrace as a culture for a greeting, you get a clean hot towel in a restaurant when you are going to eat, vs the Latin American cultures that still do the kiss hug greeting. Sapin is a kiss hug culture. France is a kiss hug culture.
For the italy ones too I bet that region was known for the kiss hug greeting, and after a while they realized it and the rest of the country stopped doing it. That would easily explain the significant differentials if one was open minded about contact.
and yes UK with their bars are open as I have mentioned in a bar drinking you make mistakes the more you drink and there are so many cross contact areas there.
Sweeden and netherlands just did nothing basically.
If you look at what I just mentioned for high contact cultures from bars to kiss hug other than the USA we probably have the top 20 highest rate nations.
dean- Posts : 5607
Join date : 2008-01-01
 Re: I do not believe it is airborn it is touch
Re: I do not believe it is airborn it is touch
my take in masks is they prevent you from touching your face directly which prevents you if you touched a contaminated surface from infecting yourself as easily. Thus when taking the mask off wash your hands first and when done removing and setting it down wash again. As noted people touch their faces over 20 times an hour as a norm. with a mask on if you touch the mask which does happen as it is peer reviewed you are not getting it into your mouth or nose.
dean- Posts : 5607
Join date : 2008-01-01
 Re: I do not believe it is airborn it is touch
Re: I do not believe it is airborn it is touch
I have been thinking about airborne vs contact and viral loads in relations to the keyboard. Considering the keyboard has one of the highest germ loads as shown in peer reviewed test after test (400 times that of a toilet seat), it is there from our hands as the we are not breathing on the keyboard, same with the light switch, doorknob, coffee pot handle, fridge handle, back of chairs, elevator button, we do not breath on those either and they are all very high in germ loads.). Would be interesting if they did a check on the keyboard vs the monitor which the monitor is what you are directly breathing on.
dean- Posts : 5607
Join date : 2008-01-01
Page 1 of 3 • 1, 2, 3 
Page 1 of 3
Permissions in this forum:
You cannot reply to topics in this forum